Complementary Lupus Care
July 30, 2012 Written by JP [Font too small?]Systemic lupus erythematosus (SLE), commonly referred to as lupus, is a chronic autoimmune disease that disproportionately affects younger women. Autoimmune diseases are characterized by an inappropriate response by the immune system which provokes an attack against healthy tissue. In the case of lupus, an inflammatory reaction occurs which can affect numerous sites in the body, including the cardiovascular system, the digestive tract and joints. The conventional management of lupus typically involves the use of anti-inflammatory drugs and corticosteroids that suppress immune function. Unfortunately, both of these pharmaceutically-based approaches carry the risk on unwanted side effects.
Alternative and complementary medicine may or may not provide adequate symptomatic relief for those living with lupus. However, there is enough scientific evidence available to at least consider and, possibly, experiment with the following natural approaches in consultation with a physician.
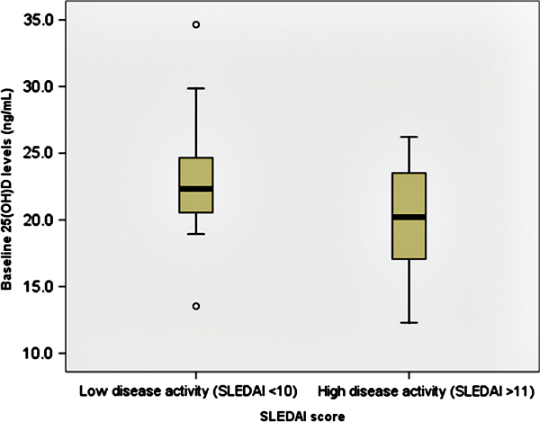
Five dietary supplements stand out as potentially beneficial options for SLE patients. 1) Higher levels of Vitamin D have been linked to lower disease activity and may likewise reduce bone loss, a common side effect of long term corticosteroid use; 2) Fish oil, in dosages of approximately 3 grams/day, “not only has a therapeutic effect on disease activity, but also improves endothelial function and reduces oxidative stress and may, therefore, confer cardiovascular benefits”; 3) 1,500 mg of turmeric daily was recently shown to protect against SLE-related high blood pressure and kidney damage; 4) Adding a ginseng extract that is standardized for ginsenosides to conventional care (prednisone) significantly improved response rates in a pilot study involving 60 adults with SLE; 5) Pycnogenol, a pine bark extract, may also work in conjunction with standard interventions to improve the efficacy of treatment and protect against various SLE health concerns such as excessive inflammation, kidney damage and oxidative stress.
Maintaining a consistent exercise regimen and managing stress are at least as important as any dietary or supplemental approaches. Although it may seem counterintuitive, exercising actually reduces fatigue in those living with lupus. Combining exercise with stress reduction is of complementary value because lowering stress addresses other key symptoms that are shared by most of those with SLE: pain perception and “psychological dysfunction”. Finally, if additional support is necessary, I would suggest looking into the viability of acupuncture. A preliminary study appearing in the December 2008 issue of Lupus reports that 40% of SLE patients receiving acupuncture, 10 sessions total, exhibited a 30% or greater decline in pain scores. The same was not true of study participants who were administered “usual care”.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Vitamin D Levels: Its Relationship to Bone Mineral Density Response … (link)
Study 2 – Serum Concentrations of 25-OH Vitamin D in Patients with Systemic … (link)
Study 3 – A Randomised Interventional Trial of ω-3-Polyunsaturated Fatty Acids … (link)
Study 4 – The Clinical Effect of Dietary Supplementation with Omega-3 Fish Oils … (link)
Study 5 – Oral Supplementation of Turmeric Decreases Proteinuria, Hematuria, … (link)
Study 6 – Efficacy of Ginsenosides Combined with Prednisone in Patients with SLE … (link)
Study 7 – Pycnogenol® Efficacy in the Treatment of Systemic Lupus … (link)
Study 8 – Effects of a Stress-Reduction Program on Psychological Function, Pain, … (link)
Study 9 – Fatigue in Systemic Lupus Erythematosus: A Randomized Controlled … (link)
Study 10 – Acupuncture for Systemic Lupus Erythematosus: A Pilot RCT Feasibility … (link)
Lower Vitamin D Is Linked to Higher Lupus Disease Activity
Source: Int J Rheum Dis. 2012 Feb;15(1):17-24. (link)
Tags: Acupuncture, Fish Oil, Lupus
Posted in Alternative Therapies, Mental Health, Nutritional Supplements

July 30th, 2012 at 8:21 pm
Hello JP,
I am very interested in this article, it is full of good info…I personally have experienced an autoimmune response, however three docs have no idea where it is coming from. I have been miserable since June 15th, and on prednisone…the urticaria is still present since that date. Lupus was one named, but ruled out. I am in limbo waiting for all results. In the meantime I stopped my Vit D,cinnamon caps, Vit c, folic acid, and multi-vite. Reason: prednisone destroys so much I felt my attempts were futile…
Do you suggest taking them? My question is not to put you on the spot, but as a matter of “am I losing out”…I appreciate your feedback.
Thanks JP, Hope you are well!
July 30th, 2012 at 11:07 pm
Hi Cynthia,
I’m really sorry to hear about your painful experience.
First and foremost, I would encourage you to never feel your efforts are futile. They are far from being that! A combination of informed choices and unshakeable confidence/faith can do wonders.
A few years back, I had (what sounds like) a similar experience. I documented it here:
https://www.healthyfellow.com/179/mangosteen-for-eczema-and-psoriasis/
I briefly looked over the list of known prednisone/supplement interactions. The supplements you’ve listed were not noted as causing any documented harm. Ideally, it would be best for you to seek out the guidance of an integrative physician who may be able to give you specific advice about which supplements would be advisable for you as a unique individual.
Do you have any hunch why these symptoms took hold when they did? Are you making any positive changes to your diet? In my experience and research, stress is often a contributing factor. Taking extra steps to lower stress is often beneficial and shouldn’t interact negatively with other conventional or holistic care.
Let’s start with that. And, just know that you can get better – sometimes it even happens faster than you’d imagine. It happened to me (or, perhaps, I made it happen) and it can for you too. Stay hopeful and strong!
Be well!
JP
August 1st, 2012 at 9:42 pm
Hello JP,
I have tried gluten free cereal, bagels, bread…I have also tried lactose free milk Other than that, my diet is very mundane. No *red meat*,I do eat chicken, veggie burgers, salads, veggies and fruits.Trader Joe’s Ice tea which I adore. I am on Zantac and Zyrtec for the anti-histamines. I do eat lots of fruit and vegetables.
Funny you mention psorasis and eczema,oh the itch is awful, I do have areas that look like psoriasis. I did see my Dermatologist and was dignosed last year with that. My frustration is that my Derm says it is not from that? It sure feels like it.
I will look into the Mangosteen and do appreciate your advice regarding this.
Will keep you informed, Thank you JP, your good sense is treasured.
Stay well
August 2nd, 2012 at 6:06 pm
Cynthia,
I don’t claim that it’ll be easy, but I would consider adopting a Paleo-style diet in addition to any alternative-, conventional care and/or supplements.
Please review the following information:
https://www.healthyfellow.com/659/dr-loren-cordain-interview-part-two/
More: https://www.healthyfellow.com/658/dr-loren-cordain-interview-part-one/
PS – IMO, many gluten-free products are far from healthy – even many of those sold in health foods stores. They’re often very high in refined carbohydrates and lack nutrient density. Please examine labels carefully and beware.
Be well!
JP
August 17th, 2015 at 8:23 pm
Updated 08/17/15:
http://onlinelibrary.wiley.com/doi/10.1002/acr.22621/abstract
Arthritis Care Res (Hoboken). 2015 May 18.
A randomized double-blind placebo-controlled trial of vitamin D supplementation in adolescents and young adults with Juvenile-onset SLE: Improvement in disease activity and fatigue scores.
PURPOSE: Vitamin D has an important immunomodulatory effect, but there are no trials that directly addressed the boosting of serum levels of 25-hydroxyvitamin D (25OHD) in Juvenile-onset Systemic Lupus Erythematosus (JoSLE). The aim of this study was to evaluate the effect of vitamin D supplementation on disease activity and fatigue in JoSLE.
METHODS: This study was a randomized double-blind placebo-controlled 24-week trial. Forty JoSLE patients were randomized (1:1) to receive oral cholecalciferol 50,000 IU/week (JoSLE-VitD) or placebo (JoSLE-PL). Medications remained stable throughout the study. Serum levels of 25OHD were measured using radioimmunoassay. Disease activity was assessed using the SLE Disease Activity Index (SLEDAI) and the European Consensus Lupus Activity Measurement (ECLAM). Fatigue was assessed using the Kids Fatigue Severity Scale (K-FSS).
RESULTS: At baseline, groups were similar regarding, age, body mass index, organ involvement, glucocorticoid dose, use of immunosuppressive drugs, SLEDAI, ECLAM, K-FSS and levels of 25OHD. After 24 weeks, the mean level of 25OHD was higher in the JoSLE-VitD group than in the JoSLE-PL (p<0.001).At the end of intervention, a significant improvement in SLEDAI (p=0.010) and a tendency for ECLAM (p=0.076) was observed in the JoSLE-VitD group compared to the JoSLE-PL. Regarding fatigue evaluation, a reduction of fatigue related to social life score was found in the JoSLE-VitD group compared to the JoSLE-PL group (p=0.008). Cholecalciferol was well tolerated with no serious adverse events.
CONCLUSION: This study suggests that cholecalciferol supplementation for 24 weeks is effective in decreasing disease activity and improving fatigue in JoSLE patients.
Be well!
JP
August 17th, 2015 at 8:26 pm
Updated 08/17/15:
http://lup.sagepub.com/content/24/4-5/499.abstract
Lupus. 2015 Apr;24(4-5):499-506.
A 24-month prospective study on the efficacy and safety of two different monthly regimens of vitamin D supplementation in pre-menopausal women with systemic lupus erythematosus.
BACKGROUND: Low vitamin D (vit.D) serum levels are common in patients with systemic lupus erythematosus (SLE) and seem to correlate with higher disease activity. We investigated the effects of different regimens of vit.D supplementation in SLE patients with inactive disease.
METHODS: This 24-month prospective study included 34 SLE women who were randomized to receive, together with their ongoing treatment, a standard regimen (SR) of cholecalcipherol (25,000 UI monthly) or an intensive regimen (IR) (300,000 UI initial bolus followed by 50,000 UI monthly) for one year and then were switched to the other regimen in the second year. Patients were seen quarterly for assessment of 25-OH vit.D levels, disease activity, SLE serology and bone metabolism markers.
RESULTS: By intra-patient comparison, only the IR was found able to significantly raise vit.D serum levels. After 12 months, values above 30 ng/ml were found in 75% of patients in IR while in only 28% in SR. No significant differences in disease activity and SLE serology were found at any time point between SR and IR. No changes in the mineral metabolism were observed.
CONCLUSIONS: The IR was safe and effective in obtaining sufficient levels of vit.D in most SLE patients. However, both regimens of supplementation did not differently affect disease activity nor SLE serology.
Be well!
JP
August 17th, 2015 at 8:28 pm
Updated 08/17/15:
http://lup.sagepub.com/content/24/4-5/483.abstract
Lupus. 2015 Apr;24(4-5):483-9.
A randomized double-blind placebo-controlled study adding high dose vitamin D to analgesic regimens in patients with musculoskeletal pain.
BACKGROUND: The current mode of therapy for many patients with musculoskeletal pain is unsatisfactory.
PURPOSE: We aimed to assess the impact of adding 4000 IU of vitamin D on pain and serological parameters in patients with musculoskeletal pain.
MATERIALS AND METHODS: This was a randomized, double-blinded and placebo-controlled study assessing the effect of 4000 IU of orally given vitamin D3 (cholecalciferol) (four gel capsules of 1000 IU, (SupHerb, Israel) vs. placebo on different parameters of pain. Eighty patients were enrolled and therapy was given for 3 months. Parameters were scored at three time points: prior to intervention, at week 6 and week 12. Visual analogue scale (VAS) scores of pain perception were recorded following 6 and 12 weeks. We also measured serum levels of leukotriene B4 (LTB4), interleukin 6 (IL-6), tumor necrosis factor alpha (TNFα) and prostaglandin E2 (PGE2) by ELISA.
RESULTS: The group receiving vitamin D achieved a statistically significant larger decline of their VAS measurement throughout the study compared with the placebo group. The need for analgesic ‘rescue therapy’ was significantly lower among the vitamin D-treated group. TNFα levels decreased by 54.3% in the group treated with vitamin D and increased by 16.1% in the placebo group. PGE2 decreased by39.2% in the group treated with vitamin D and increased by 16% in the placebo group. LTB4 levels decreased in both groups by 24% (p < 0.05). CONCLUSION: Adding 4000 IU of vitamin D for patients with musculoskeletal pain may lead to a faster decline of consecutive VAS scores and to a decrease in the levels of inflammatory and pain-related cytokines. Be well! JP
August 20th, 2015 at 7:04 pm
Updated 08/20/15:
http://www.nutritionj.com/content/14/1/82
Nutr J. 2015 Aug 18;14(1):82.
Placebo-controlled randomized clinical trial of fish oil’s impact on fatigue, quality of life, and disease activity in Systemic Lupus Erythematosus.
INTRODUCTION: A recent metabolomic screen of sera from patients with Systemic Lupus Erythematosus (SLE) found reduction of antioxidants and substrates for energy generation. These metabolic alterations may underlie one of the most common features of SLE – fatigue. The metabolomic studies also noted reduced omega-3 fatty acids, which are powerful anti- oxidants. This deficiency may be causally related to oxidative stress, inflammation, disease activity, and fatigue in SLE. Supplementation of omega-3 fatty acids using fish oil in SLE has been shown to reduce oxidative stress in other studies. The objective of this study is to evaluate the effect of fish oil supplementation on clinical measures of fatigue, quality of life, and disease activity as part of a randomized clinical trial.
METHODS: Fifty SLE patients recruited in outpatient clinics were randomized 1:1 to fish oil supplementation or olive oil placebo, and blinded to their treatment group. At baseline and after 6 months of treatment, RAND Short Form-36 (RAND SF-36), Fatigue Severity Scale (FSS), SLE Disease Activity Index (SLEDAI), and Physician Global Assessment (PGA) were completed; serum was also collected for soluble mediator analysis.
RESULTS: Thirty-two patients completed the study. PGA improved significantly in the fish oil group compared with the placebo group (p = 0.015). The RAND SF-36 Energy/fatigue and Emotional well-being scores demonstrated improvement trends (p = 0.092 and 0.070). No clear difference was seen in FSS and SLEDAI (p = 0.350 and p = 0.417). Erythrocyte sedimentation rate and serum IL-12 were reduced (p = 0.008 and p = 0.058); while serum IL-13 was increased by fish oil supplementation (p = 0.033).
CONCLUSIONS: In this randomized, placebo-controlled 6-month trial, SLE patients randomized to fish oil supplementation demonstrated improvement in their PGA, RAND SF-36, and some circulating inflammatory markers.
Be well!
JP
December 31st, 2017 at 5:49 pm
Updated 12/31/17:
http://www.sciencedirect.com/science/article/pii/S2255502116300815?via%3Dihub
Rev Bras Reumatol Engl Ed. 2017 Nov – Dec;57(6):526-534.
Omega-3 fatty acids, inflammatory status and biochemical markers of patients with systemic lupus erythematosus: a pilot study.
BACKGROUND: Studies have shown that omega-3 fatty acids reduce the concentrations of eicosanoids, cytokines, chemokines, C-reactive protein (CRP) and other inflammatory mediators.
OBJECTIVE: To investigate the effects of omega-3 fatty acids on circulating levels of inflammatory mediators and biochemical markers in women with systemic lupus erythematosus (SLE).
METHODS: Experimental clinical study (clinical trial: NCT02524795); 49 women with SLE (ACR1982/1997) were randomized: 22 to the omega-3 group (daily intake of 1080mg EPA+200mg DHA, for 12 weeks) and 27 to the control group. The inflammatory mediators and biochemical markers at T0 and T1 in omega-3 group were compared using Wilcoxon test. U-Mann-Whitney test was used to compare variations of measured variables [ΔV=pre-treatment (T0)-post-treatment (T1) concentrations] between groups. p<0.05 was considered significant.
RESULTS: The median (interquartile range - IQR) of age was 37 (29-48) years old, of disease duration was 7 (4-13) years, and of SLEDAI-2K was 1 (0-2). The median (IQR) of variation in CRP levels between the two groups showed a decrease in omega-3 group while there was an increase in control group (p=0.008). The serum concentrations of IL-6 and IL-10, leptin and adiponectin did not change after a 12 week treatment.
CONCLUSIONS: Supplementation with omega-3 had no impact on serum concentrations of IL-6, IL-10, leptin and adiponectin in women with SLE and low disease activity. There was a significant decrease of CRP levels as well as evidence that omega-3 may impact total and LDL-cholesterol.
Be well!
JP
January 1st, 2018 at 6:31 pm
Updated 1/1/18:
http://www.sciencedirect.com/science/article/pii/S2255502117300548?via%3Dihub
Rev Bras Reumatol Engl Ed. 2017 Sep – Oct;57(5):466-471.
Effect of vitamin D supplementation on patients with systemic lupus erythematosus: a systematic review.
The objective of this systematic review was to analyze clinical trials carried out for the investigation of the effect of vitamin D supplementation on systemic lupus erythematosus. The research was performed from August to September 2016, without limits regarding year of publication, restriction of gender, age, and ethnicity. For the guiding question, the PICO strategy was employed. To evaluate the quality of the publications the PRISMA protocol and Jadad scale were used. The risk of bias analysis of the clinical trials was performed using the Cochrane collaboration tool. After the process of article selection and removal of duplicates, four articles were identified as eligible. The results of three studies showed a positive effect of supplementation on disease activity reduction and significant improvement in levels of inflammatory markers, fatigue, and endothelial function. Only one study showed no improvement in disease activity after supplementation. Moreover, all studies showed an increase in serum vitamin D levels. The data from this review provide evidence on the benefits of vitamin D supplementation in patients with lupus and vitamin D insufficiency/deficiency. However, it is still necessary to elucidate whether vitamin D acts in the protection against this metabolic disorder, as well as the standardization of the type, dose and time of vitamin D supplementation.
Be well!
JP
January 3rd, 2018 at 11:26 pm
Updated 1/3/18:
http://onlinelibrary.wiley.com/doi/10.1002/ptr.5827/abstract
Phytother Res. 2017 Jul;31(7):1063-1071.
A Randomized, Double-blind, Placebo-controlled Clinical Trial Examining the Effects of Green Tea Extract on Systemic Lupus Erythematosus Disease Activity and Quality of Life.
Antiinflammatory and immunomodulatory benefit of green tea (Camellia sinensis) in autoimmune disease has been proven in recent studies. The objective of this study was to assess the effects of green tea on disease activity and quality of life in systemic lupus erythematosus patients. A randomized controlled trial on subjects with lupus was conducted, and 68 patients in the age range of 39.1 ± 10.3 years and body mass index of 25.7 ± 5.21 kg/m2 completed the 12-week study. Patients were randomly divided into two groups of intervention (1000 mg green tea extract, two capsules/day) and control (1000 mg of starch, two capsules/day). Main outcome measure, systemic lupus erythematosus disease activity, was assessed by the systemic lupus erythematosus disease activity index at the first and after 3 months of intervention. In addition, patient’s quality of life was evaluated by short form of quality-of-life questionnaire at baseline and after 3 months. Green tea extract supplementation significantly reduced disease activity in lupus patients (p < 0.004); in addition, it significantly increased the vitality (p < 0.006) and general health (p < 0.01). This study showed that daily consumption of green tea extracts for 12 weeks improves the systemic lupus erythematosus disease activity as well as some aspects of quality of life. Be well! JP
January 16th, 2018 at 1:12 am
Updated 1/15/18:
http://onlinelibrary.wiley.com/doi/10.1111/eci.12885/abstract
Eur J Clin Invest. 2018 Jan 10.
Cardiorespiratory fitness and age-related arterial stiffness in lupus.
BACKGROUND: The aim of the present study was twofold: 1) to examine the association of cardiorespiratory fitness with arterial stiffness in women with systemic lupus erythematosus; 2) to assess the potential interaction of cardiorespiratory fitness with age on arterial stiffness in this population.
MATERIALS AND METHODS: A total of 49 women with systemic lupus erythematosus (mean age 41.3 [Standard deviation 13.8] years) and clinical stability during the previous 6 months were included in the study. Arterial stiffness was assessed through pulse wave velocity (Mobil-O-Graph® 24h pulse wave velocity monitor). Cardiorespiratory fitness was estimated with the Siconolfi step test and the six-minute walk test.
RESULTS: Cardiorespiratory fitness was inversely associated with pulse wave velocity in crude analyses (P<0.05), although this relationship was attenuated when age and other cardiovascular risk factors were controlled. There was a cardiorespiratory fitness×age interaction effect on pulse wave velocity, regardless of the test used to estimate cardiorespiratory fitness (P<0.001 for the Siconolfi step test; P=0.005 for the six-minute walk test), indicating that higher cardiorespiratory fitness was associated with a lower increase in pulse wave velocity per each year increase in age.
CONCLUSIONS: The results of the present study suggest that cardiorespiratory fitness attenuates the age-related arterial stiffening in women with systemic lupus erythematosus and might thus contribute to the primary prevention of cardiovascular disease in this population. Since the cross-sectional design precludes establishing causal relationships, future clinical trials should confirm or contrast these findings.
Be well!
JP