Triglyceride Heart Risk
November 25, 2013 Written by JP [Font too small?]For years, I’ve been telling my clients and physician friends that the current obsession with cholesterol levels is way out of focus. In my opinion, high LDL (aka “bad”) cholesterol is more likely than not a very small contributor to the current epidemic of cardiovascular disease. On the other hand, elevated triglycerides appear to be a far better marker for lifestyle choices which probably affect heart disease and stroke risk. Fortunately, a few, simple dietary changes can lower high triglycerides and significantly improve cardiovascular wellness. Best of all, lowering hypertriglyceridemia often doesn’t require any medications or supplements.
Triglycerides are a form of fat that is contained in blood. Elevated levels of blood triglycerides (over 150 mg/dL) have been implicated in a higher risk of cardiovascular disease and all-cause mortality. In fact, a recent review of 61 studies found that the risk of death increased incrementally in relation to the amount of triglycerides present in blood samples of over 1,000,000 study participants. Simply put, the higher the level of triglycerides, the greater the incidence of cardiovascular and overall mortality.
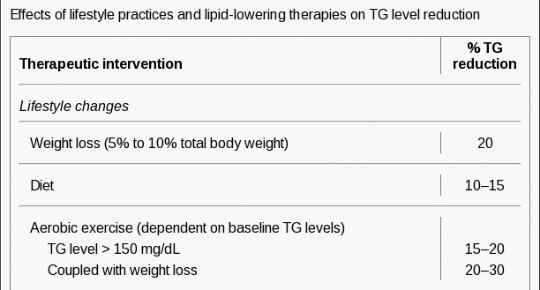
Interestingly, conventional medicine frequently employs a distinctly natural approach to managing hypertriglyceridemia: high dosage, prescription fish oil. However, many people with high triglycerides may want to consider dietary interventions prior to (or in conjunction with) prescription or supplemental fish oil therapy. The medical literature informs that eating plenty of green leafy vegetables, nuts and oily fish can dramatically lower blood triglycerides. What’s more, if you consistently replace high glycemic carbohydrates (refined, starchy and sugary foods) with fatty fish, greens and nuts, your triglycerides levels will likely plummet. If additional support is required, losing excess weight and regular aerobic exercise can further affect triglyceride concentrations and improve your overall lipid profile. Best of all, these three nutritional strategies tend to support virtually every aspect of wellness without side effects.
My Top 3 Green Leafy Vegetables: Kale, Spinach and Swiss Chard
Dosage: 2 or more servings daily
My Top 3 Nuts: Almonds, Pistachios and Walnuts
Dosage: 1 – 3 ounces daily
My Top 3 Fish: (Wild) Black Cod, Sardines, Wild Alaskan Salmon
Dosage: 2 – 5 servings weekly
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Effects of Blood Triglycerides on Cardiovascular and All-Cause Mortality … (link)
Study 2 – Lifestyle Modifications for Treatment of Hypertriglyceridemia … (link)
Study 3 – Habitual Diets Rich in Dark-Green Vegetables Are Associated with … (link)
Study 4 – Effects of Total and Green Vegetable Intakes on Glycated Hemoglobin … (link)
Study 5 – Effect of Ketogenic Mediterranean Diet w/ Phytoextracts and Low … (link)
Study 6 – Inclusion of Atlantic Salmon in the Chinese Diet Reduces Cardiovascular … (link)
Study 7 – Inclusion of Fish or Fish Oil in Weight-Loss Diets for Young Adults ... (link)
Study 8 – Benefits of Salmon Eating on Traditional & Novel Vascular Risk Factors … (link)
Study 9 – A Randomized Trial of the Effects of an Almond-Enriched, Hypocaloric … (link)
Study 10 – Pistachio Nuts Reduce Triglycerides & Body Weight by Comparison to … (link)
Natural Ways to Lower Triglycerides
Source: Curr Cardiol Rep. 2011 Dec;13(6):544-52. (link)
Tags: Fish, Nuts, Vegetables
Posted in Food and Drink, Heart Health, Nutrition


December 1st, 2013 at 3:14 pm
“In my opinion, high LDL (aka “bad”) cholesterol is more likely than not a very small contributor to the current epidemic of cardiovascular disease.”
Why so?
Also-what is your opinion on LDL-P/ApoB?
December 2nd, 2013 at 4:11 pm
Hi Charles,
IMO, overemphasizing the importance of LDL cholesterol is much like counting the number of $1 bills in a wallet and, based on the value, trying to extrapolate one’s financial status. It’s a micro issue that has been inappropriately magnified.
My best advice is not to rely on any one test to guide your cardiovascular wellness protocol. Having said that, blood pressure and sugar are important and can be easily monitored. Daily stress management and exercise almost certainly help. So too does constructive social interaction and volunteerism. Eating a Mediterranean-style diet, particularly one low in carbohydrates, has been proven to reduce various (likely) risk factors for CVD (blood pressure, blood sugar, inflammation, LDL cholesterol, triglycerides, waist circumference, etc.). So, rather than relying heavily on conventional and “up-and-coming” tests, I typically recommend adopting diet and lifestyle approaches which are associated with improved cardiovascular function and mortality.
A few relevant links:
https://www.healthyfellow.com/1524/kale-kimchi-cholesterol-reducer/
https://www.healthyfellow.com/1273/dr-stephen-sinatra-interview-part-one/
https://www.healthyfellow.com/1276/dr-stephen-sinatra-interview-%E2%80%93-part-two/
https://www.healthyfellow.com/1062/dr-jonny-bowden-interview-part-one/
https://www.healthyfellow.com/1065/dr-jonny-bowden-interview-part-two/
Be well!
JP
December 4th, 2013 at 6:31 pm
JP
Your thoughts on this from Dr Thomas Dayspring
http://www.lecturepad.org/dayspring/lipidaholics/pdf/LipidaholicsCase291.pdf
Let’s get rid of the nonsense seen all over the internet that atherosclerosis is an inflammatory disease, not a cholesterol disease. That is baloney-with the reality being that it is both. One cannot have atherosclerosis without sterols, predominantly cholesterol being in the artery wall: No cholesterol in arteries – no atherosclerosis. Plenty of folks have no systemic vascular inflammation and have atherosclerotic plaque. However clinicians have no test that measures cholesterol within the plaque – it is measured in the plasma. It is assumed, that if total or LDL-C or non-HDL-C levels are elevated the odds are good that some of that cholesterol will find its way into the arteries, and for sure there, are many studies correlating those measurements with CHD risk. Yet, we have lots of patients with very low TC and LDL-C who get horrific atherosclerosis. We now recognize that the cholesterol usually gains arterial entry as a passenger inside of an apoB-containing lipoprotein (the vast majority of which are LDLs) and the primary factor driving LDL entry into the artery is particle number (LDL-P), not particle cholesterol content (LDL-C). Because the core lipid content of each and every LDL differs (how many cholesterol molecules it traffics) it takes different numbers of LDLs to traffic a given number of cholesterol molecules: the more depleted an LDL is of cholesterol, the more particles (LDL-P) it will take to carry a given cholesterol mass (LDL-C). The usual causes of cholesterol depleted particles are that the particles are small or they are TG-rich and thus have less room to carry cholesterol molecules. Who has small LDLs or TG-rich LDL’s? – insulin resistant patients! After particle number endothelial integrity is certainly related to atherogenic particle entry: inflamed endothelia have inter-cellular gaps and express receptors that facilitate apoB-particle entry. So the worse scenario is to have both high apoB and an inflamed dysfunctional endothelium. Is it better to have no inflammation in the endothelium – of course! But make no mistake the driving force of atherogenesis is entry of apoB particles and that force is driven primarily by particle number not arterial wall inflammation: please see Ira Tabas, Kevin Jon Williams, Jan Borén. Subendothelial Lipoprotein Retention as the Initiating Process in Atherosclerosis Update and Therapeutic Implications Circulation. 2007;116:1832-44.
http://circ.ahajournals.org/content/116/16/1832.full
December 7th, 2013 at 1:38 am
Hi Charles,
I agree that endothelial integrity and insulin resistance both factor into CVD. Other likely factors include hypertensive-related damage, imbalanced omega-3/6 fatty acids, oxidized cholesterol and many more. However, rather than focusing on the latest and greatest markers and tests, I think it’s preferable to pursue dietary and lifestyle choices which tend to promote various aspects of wellness including connective tissue integrity, insulin sensitivity, low systemic inflammation and beyond.
A recent case in point:
http://atvb.ahajournals.org/content/early/2013/11/27/ATVBAHA.113.302327.abstract
Be well!
JP
March 1st, 2015 at 11:28 pm
Update: Low carb diets are an effective way to lower triglycerides …
http://annals.org/article.aspx?articleid=1900694
Ann Intern Med. 2014 Sep 2;161(5):309-18. doi: 10.7326/M14-0180.
Effects of low-carbohydrate and low-fat diets: a randomized trial.
BACKGROUND: Low-carbohydrate diets are popular for weight loss, but their cardiovascular effects have not been well-studied, particularly in diverse populations.
OBJECTIVE: To examine the effects of a low-carbohydrate diet compared with a low-fat diet on body weight and cardiovascular risk factors.
DESIGN: A randomized, parallel-group trial. (ClinicalTrials.gov: NCT00609271).
SETTING: A large academic medical center.
PARTICIPANTS: 148 men and women without clinical cardiovascular disease and diabetes.
INTERVENTION: A low-carbohydrate (<40 g/d) or low-fat (<30% of daily energy intake from total fat [<7% saturated fat]) diet. Both groups received dietary counseling at regular intervals throughout the trial.
MEASUREMENTS: Data on weight, cardiovascular risk factors, and dietary composition were collected at 0, 3, 6, and 12 months.
RESULTS: Sixty participants (82%) in the low-fat group and 59 (79%) in the low-carbohydrate group completed the intervention. At 12 months, participants on the low-carbohydrate diet had greater decreases in weight (mean difference in change, -3.5 kg [95% CI, -5.6 to -1.4 kg]; P = 0.002), fat mass (mean difference in change, -1.5% [CI, -2.6% to -0.4%]; P = 0.011), ratio of total-high-density lipoprotein (HDL) cholesterol (mean difference in change, -0.44 [CI, -0.71 to -0.16]; P = 0.002), and triglyceride level (mean difference in change, -0.16 mmol/L [-14.1 mg/dL] [CI, -0.31 to -0.01 mmol/L {-27.4 to -0.8 mg/dL}]; P = 0.038) and greater increases in HDL cholesterol level (mean difference in change, 0.18 mmol/L [7.0 mg/dL] [CI, 0.08 to 0.28 mmol/L {3.0 to 11.0 mg/dL}]; P < 0.001) than those on the low-fat diet. LIMITATION: Lack of clinical cardiovascular disease end points. CONCLUSION: The low-carbohydrate diet was more effective for weight loss and cardiovascular risk factor reduction than the low-fat diet. Restricting carbohydrate may be an option for persons seeking to lose weight and reduce cardiovascular risk factors. Be well! JP
March 5th, 2015 at 2:00 pm
Update: Fish oil may reduce damage caused by heart attack …
http://www.webmd.com/heart/news/20150304/omega-3-fatty-acids-may-stem-further-damage-after-heart-attack
“WEDNESDAY, March 4, 2015 (HealthDay News) — High doses of omega-3 fatty acids may protect against further damage in heart attack patients, a preliminary study suggests.
The research included 374 heart attack survivors who received standard treatment and took either a 4-gram prescription-only dose of omega-3 fatty acids each day or a placebo. The researchers said that people probably couldn’t get that level of omega-3 fatty acids from diet alone. To illustrate how large a dose that is, the researchers noted that 4 grams of omega-3 fatty acids is the equivalent of eating 8 ounces of salmon.
Using MRIs, the patients’ hearts were scanned two weeks, four weeks and six months after their heart attack.
Compared to those taking the placebo, patients taking the omega-3 capsules had lower levels of inflammation and were 39 percent less likely to show deterioration of heart function. There was also less thickening or scarring of the areas of the heart that were not directly damaged during the heart attack. This thickening, also known as fibrosis, often develops when the surviving heart muscle works harder to compensate for the damaged tissue, according to the researchers.”
Be well!
JP
April 28th, 2015 at 11:29 am
Update 04/28/15:
http://jn.nutrition.org/content/early/2015/04/22/jn.114.203190.abstract
J Nutr. 2015 Apr 22. pii: jn203190.
Cranberry Juice Consumption Lowers Markers of Cardiometabolic Risk, Including Blood Pressure and Circulating C-Reactive Protein, Triglyceride, and Glucose Concentrations in Adults.
BACKGROUND: Cardiometabolic risk is the risk of cardiovascular disease (CVD), diabetes, or stroke, which are leading causes of mortality and morbidity worldwide.
OBJECTIVE: The objective of this study was to determine the potential of low-calorie cranberry juice (LCCJ) to lower cardiometabolic risk.
METHODS: A double-blind, placebo-controlled, parallel-arm study was conducted with controlled diets. Thirty women and 26 men (mean baseline characteristics: 50 y; weight, 79 kg; body mass index, 28 kg/m2) completed an 8-wk intervention with LCCJ or a flavor/color/energy-matched placebo beverage. Twice daily volunteers consumed 240 mL of LCCJ or the placebo beverage, containing 173 or 62 mg of phenolic compounds and 6.5 or 7.5 g of total sugar per a 240-mL serving, respectively.
RESULTS: Fasting serum triglycerides (TGs) were lower after consuming LCCJ and demonstrated a treatment × baseline interaction such that the participants with higher baseline TG concentrations were more likely to experience a larger treatment effect (1.15 ± 0.04 mmol/L vs. 1.25 ± 0.04 mmol/L, respectively; P = 0.027). Serum C-reactive protein (CRP) was lower for individuals consuming LCCJ than for individuals consuming the placebo beverage [ln transformed values of 0.522 ± 0.115 ln(mg/L) vs. 0.997 ± 0.120 ln(mg/L), P = 0.0054, respectively, and equivalent to 1.69 mg/L vs. 2.71 mg/L back-transformed]. LCCJ lowered diastolic blood pressure (BP) compared with the placebo beverage (69.2 ± 0.8 mm Hg for LCCJ vs. 71.6 ± 0.8 mm Hg for placebo; P = 0.048). Fasting plasma glucose was lower (P = 0.03) in the LCCJ group (5.32 ± 0.03 mmol/L) than in the placebo group (5.42 ± 0.03 mmol/L), and LCCJ had a beneficial effect on homeostasis model assessment of insulin resistance for participants with high baseline values (P = 0.035).
CONCLUSION: LCCJ can improve several risk factors of CVD in adults, including TGs, CRP, glucose, insulin resistance, and diastolic BP.
Be well!
JP
May 18th, 2015 at 4:49 pm
Update 05/18/15:
http://www.nrjournal.com/article/S0271-5317%2815%2900097-4/abstract
Nutrition Research – May 13, 2015
Paleolithic nutrition improves plasma lipid concentrations of hypercholesterolemic adults to a greater extent than traditional heart-healthy dietary recommendations
Recent research suggests that traditional grain-based heart healthy diet recommendations, which replace dietary saturated fat with carbohydrate and reduce total fat intake, may result in unfavorable plasma lipid ratios, with reduced high-density lipoprotein (HDL) and an elevation of low-density lipoprotein (LDL) and triacylglycerols (TG). The current study tested the hypothesis that a grain-free Paleolithic diet would induce weight loss and improve plasma total cholesterol (TC), HDL, LDL and TG concentrations in non-diabetic adults with hyperlipidemia to a greater extent than a grain-based heart healthy diet, based on the recommendations of the American Heart Association. Twenty volunteers (10 male, 10 female) aged 40 to 62 years were selected based on diagnosis of hypercholesterolemia. Volunteers were not taking any cholesterol-lowering medications and adhered to a traditional heart healthy diet for four months, followed by a Paleolithic diet for four months. Regression analysis was used to determine whether change in body weight contributed to observed changes in plasma lipid concentrations. Differences in dietary intakes and plasma lipid measures were assessed using repeated measures ANOVA. Four months of Paleolithic nutrition significantly lowered (P < 0.001) mean TC, LDL, and TG and increased (P < 0.001) HDL, independent of changes in body weight, relative to both baseline and the traditional heart healthy diet. Paleolithic nutrition offers promising potential for nutritional management of hyperlipidemia in adults whose lipid profiles have not improved after following more traditional heart healthy dietary recommendations. Be well! JP
May 28th, 2015 at 6:33 pm
Update 05/28/15:
http://www.nmcd-journal.com/article/S0939-4753%2815%2900119-2/abstract
Nutrition, Metabolism and Cardiovascular Diseases – May 13, 2015
The triglyceride-lowering effect of supplementation with dual probiotic strains, Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032: reduction of fasting plasma lysophosphatidylcholines in nondiabetic and hypertriglyceridemic subjects
Background and Aims: This study evaluated the triglyceride (TG)-lowering effects of consuming dual probiotic strains of Lactobacillus curvatus (L. curvatus) HY7601 and Lactobacillus plantarum (L. plantarum) KY1032 on the fasting plasma metabolome.
Methods and Results: A randomized, double-blind, placebo-controlled study was conducted on 92 participants with hypertriglyceridemia but without diabetes. Over a 12-week testing period, the probiotic group consumed 2 g of powder containing 5 x 109 colony-forming units (cfu) of L. curvatus HY7601 and 5 x 109 cfu of L. plantarum KY1032 each day, whereas the placebo group consumed the same product without probiotics. Fasting plasma metabolomes were profiled using UPLC-LTQ-Orbitrap MS. After 12 weeks of treatment, the probiotic group displayed a 20% reduction (p = 0.001) in serum TGs and 25% increases (p = 0.001) in apolipoprotein A-V (apoA-V). At the 12-week follow-up assessment, the following 11 plasma metabolites were significantly reduced in the probiotic group than the placebo group: palmitoleamide, palmitic amide, oleamide, and lysophosphatidyl choline (lysoPC) containing C14:0, C16:1, C16:0, C17:0, C18:3, C18:2, C18:1, and C20:3. In the probiotic group, changes (△) in TG were negatively correlated with △ apoA-V, which were positively correlated with △ FFA. In addition, △ FFA was strongly and positively correlated with △ lysoPCs in the probiotic group but not the placebo group.
Conclusions: The triglyceride-lowering effects of probiotic supplementation, partly through elevated apoA-V, in borderline to moderate hypertriglyceridemic subjects showed reductions in plasma metabolites; fatty acid primary amides and lysoPCs (NCT02215694; http://www.clinicaltrials.gov).
Be well!
JP
September 3rd, 2015 at 4:49 pm
Updated 09/03/15:
http://www.foodandnutritionresearch.net/index.php/fnr/article/view/27651
Food Nutr Res. 2015 Aug 19;59:27651.
Effect of a high intake of cheese on cholesterol and metabolic syndrome: results of a randomized trial.
BACKGROUND: Cheese is generally rich in saturated fat, which is associated with increased risk for cardiovascular diseases. Nevertheless, recent reports suggest that cheese may be antiatherogenic.
OBJECTIVE: The goal of this study was to assess whether intake of two types of Norwegian cheese, with widely varying fat and calcium content, might influence factors of the metabolic syndrome and serum cholesterol levels differently.
DESIGN: A total of 153 participants were randomized to one of three groups: Gamalost(®), a traditional fat- and salt-free Norwegian cheese (50 g/day), Gouda-type cheese with 27% fat (80 g/day), and a control group with a limited cheese intake. Blood samples, anthropometric measurements, blood pressure, and questionnaires about lifestyle and diet were obtained at inclusion and end.
RESULTS: At baseline, there were no differences between the groups in relevant baseline characteristics, mean age 43, 52.3% female. After 8 weeks’ intervention, there were no changes in any of the metabolic syndrome factors between the intervention groups compared with the control group. There were no increases in total- or LDL cholesterol in the cheese groups compared with the control. Stratified analysis showed that those in the Gouda group with metabolic syndrome at baseline had significant reductions in total cholesterol at the end of the trial compared with control (-0.70 mmol/L, p=0.013), and a significantly higher reduction in mean triglycerides. In the Gamalost group, those who had high total cholesterol at baseline had a significant reduction in total cholesterol compared with control (-0.40 mmol/L, p=0.035).
CONCLUSIONS: In conclusion, cholesterol levels did not increase after high intake of 27% fat Gouda-type cheese over 8 weeks’ intervention, and stratified analysis showed that participants with metabolic syndrome had reduced cholesterol at the end of the trial.
Be well!
JP
September 23rd, 2015 at 10:07 am
Updated 09/23/15:
http://www.metabolismjournal.com/article/S0026-0495%2815%2900216-4/abstract
Metabolism. 2015 Jul 30.
Effects of pistachios on the lipid/lipoprotein profile, glycemic control, inflammation, and endothelial function in type 2 diabetes: A randomized trial.
OBJECTIVE: The health benefits of regular nut consumption have been well-documented; however, effects on cardiovascular risk in diabetes are emerging. This study examined the effects of daily pistachio consumption on the lipid/lipoprotein profile, glycemic control, markers of inflammation, and endothelial function in adults with type 2 diabetes.
MATERIALS/METHODS: We enrolled 30 adults (40-74years) with well-controlled type 2 diabetes (mean glycated hemoglobin 6.2%) in a randomized, crossover, controlled feeding study. After a 2-week run-in period, participants consumed nutritionally-adequate diets with pistachios (contributing 20% of total energy) or without pistachios for 4weeks each, separated by a 2-week washout. We assessed fasting lipids/lipoproteins, glycemic measures (while fasted and during a 75g oral glucose tolerance test), inflammatory markers, and endothelial function after each diet period.
RESULTS: Total cholesterol and the ratio of total to HDL cholesterol were significantly lower (p<0.05) following the pistachio diet (4.00mmol/L and 4.06mmol/L, respectively) compared to the control diet (4.15mmol/L and 4.37mmol/L, respectively). Triglycerides were significantly lower (p=0.003) following the pistachio diet (1.56mmol/L) compared to the control diet (1.84mmol/L). There were no treatment differences in fasting glucose and insulin, but fructosamine was significantly lower (p=0.03) following the pistachio diet (228.5μmol/l) compared to the control diet (233.5μmol/l). Inflammatory markers and endothelial function were unchanged.
CONCLUSION: Daily pistachio consumption can improve some cardiometabolic risk factors in adults with well-controlled type 2 diabetes. Our findings support recommendations that individuals with diabetes follow healthy dietary patterns that include nuts.
Be well!
JP
October 12th, 2015 at 6:17 pm
Updated 10/12/15:
http://www.ncbi.nlm.nih.gov/pubmed/26434249
J Med Assoc Thai. 2015 Jul;98 Suppl 6:S41-7.
Effect of Andrographis paniculata Extract on Triglyceride Levels of the Patients with Hypertriglyceridemia: A Randomized Controlled Trial.
BACKGROUND: Hypertriglyceridemia is one of the risk factors for cardiovascular disease, and reduction oftriglyceride (TG) level is recommended in clinical practice guidelines for the treatment. Recently, andrographolide, a main active compound of Andrographispaniculata has been shown to possess hypolipidemic effects in animals.
OBJECTIVE: To investigate the TG-lowering effects of A. paniculata extract (APE) in patients with hypertriglyceridemia (TG ≥ 150 mg/dL) using gemfibrozil treatment as the reference.
MATERIAL AND METHOD: A randomized controlled clinical trial was carried out in sixty subjects with hypertriglyceridemia. They were divided into three groups and treated with low dose of APE (APE-L, andrographolide 71.64-72.36 mg/day), high dose of APE (APE-H, andrographolide 119.64-120.36 mg/day), and gemfibrozil 300 mg/day. The treatments were conducted for 8 weeks. Guidance on lifestyle modifications was provided.
RESULTS: The primary endpoint was the mean difference ± SD (95% CI) in TG levels (baseline from the end of treatment), which were -3 ± 125.6 (-59.1, 58.5), 41.6 ± 86.3 (1.2, 82), and 57.1 ± 94.9 (12.7, 101.6) in the APE-L, APE-H, and gemfibrozil groups, respectively. APE-H 120 mg/day and gemfibrozil 300 mg/day caused a significant reduction of TG level (P = 0.0442 and 0.0145, respectively) when compared to the baseline. There was no notable difference in the safety or tolerability among the treatment groups.
CONCLUSION: In patients with modest hypertriglyceridemia with lifestyle intervention, APE-H reduced the TG level comparable to the effect of gemfibrozil 300 mg/day. APE treatment was as tolerable as gemfibrozil treatment. Hence, Andrographis paniculata might be used as an alternative medicine in treating hypertriglyceridemic patients.
Be well!
JP
December 22nd, 2015 at 2:42 pm
Updated 12/22/15:
http://www.lipidjournal.com/article/S1933-2874%2815%2900368-2/abstract
J Clin Lipidol. 2015 Nov-Dec;9(6):770-7.
Effect of DHA-rich fish oil on PPARγ target genes related to lipid metabolism in type 2 diabetes: A randomized, double-blind, placebo-controlled clinical trial.
BACKGROUND: The beneficial effects of omega-3 polyunsaturated fatty acids on lipid levels are well documented. However, the related molecular mechanisms are widely unknown. Omega-3 polyunsaturated fatty acids are natural ligand for peroxisome proliferator-activated receptor γ (PPARγ).
OBJECTIVE: The aim of this study was to evaluate the effect of docosahexaenoic acid (DHA)-rich fish oil supplementation on modulation of some PPARγ-responsive genes related to lipid metabolism.
METHODS: Patients with type 2 diabetes were randomly assigned to consume either DHA-rich fish oil (containing 2400 mg/d fish oil; DHA: 1450 mg and eicosapentaenoic acid: 400 mg) or placebo for 8 weeks. Lipid profile and glycemic control parameters as well as the gene expression of PPARγ, liver x receptor-a, ATP-binding cassette A1, and CD36 in peripheral blood mononuclear cells were measured at baseline and after 8 weeks.
RESULTS: DHA-rich fish oil supplementation resulted in decreased triglycerides (TG) level compared with placebo group, independently of the baseline value of TG (all patients (P = .003), hypertriglyceridemic subjects (P = .01), and normotriglyceridemic subjects (P = .02)). Moreover, a higher reduction in TG level was observed in hypertriglyceridemic subjects, comparing to normotriglyceridemic subjects with DHA-rich fish oil supplementation (P = .01). Other lipid parameters as well as the expression of PPARγ, liver x receptor-a, ATP-binding cassette A1, and CD36 were not affected by DHA-rich fish oil supplementation. Only in hypertriglyceridemic subjects, DHA-rich fish oil supplementation upregulated CD36 expression, compared with the placebo group (P = .01).
CONCLUSIONS: DHA-rich fish oil supplementation for 8 weeks increased CD36 expression in hypertriglyceridemic subjects, which might result to higher reduction in TG level, comparing with normotriglyceridemic subjects. However, this finding should be investigated in further studies.
Be well!
JP
May 25th, 2016 at 6:03 pm
Updated 05/25/16:
http://lipidworld.biomedcentral.com/articles/10.1186/s12944-016-0266-8
Lipids Health Dis. 2016 May 18;15(1):97.
Triglycerides are a predictive factor for arterial stiffness: a community-based 4.8-year prospective study.
BACKGROUND: Epidemiological studies have disclosed an independent effect of triglycerides on coronary heart disease despite achievement of low-density lipoprotein cholesterol goals with statin therapy. Arterial stiffness has been increasingly recognized as a strong predictor of cardiovascular disease and atherosclerotic disease. The association between triglycerides and arterial stiffness is not well characterized. We aimed to determine the relationship between triglycerides and arterial stiffness in a community-based longitudinal sample from Beijing, China.
METHODS: We related levels of plasma TGs to measures of arterial stiffness (carotid-femoral pulse wave velocity [PWV] and carotid-radial PWV) in 1447 subjects (mean age, 61.3 years) from a community-based population in Beijing, China.
RESULTS: After a median follow-up interval of 4.8 years, multiple linear regression analysis revealed that TGs were independently associated with carotid-femoral PWV (β = 0.747, P < 0.001) and carotid-radial PWV (β = 0.367, P = 0.001). In the group older than 65 years, the association between baseline TG levels and follow-up carotid-femoral PWV (β = 1.094, P = 0.001) and carotid-radial PWV (β = 0.524, P = 0.002) were strengthened. In forward stepwise multivariate logistic regression analysis, every SD increase in TGδ was associated with a 1.296-increased likelihood of the presence of carotid-femoral PWVδII (OR [per SD increase in TGδ]: 1.296; 95 % CI: 1.064 ~ 1.580; P = 0.010) in Model 2, whereas the relationship between TGδ and carotid-radial PWVδII disappeared. In addition, the relationship was strengthened between TGδ and the presence of carotid-femoral PWVδII (OR 1.526, 95 % CI: 1.088-2.141, P = 0.014) in the group older than 65 years but not carotid-radial PWVδII. No association was noted in subjects younger than 65 years. CONCLUSIONS: Lower triglyceride levels were significantly associated with decreases in carotid-femoral PWV, indicating that achieving low TG levels may be an additional therapeutic consideration in subjects with atherosclerotic disease. Be well! JP
November 30th, 2016 at 3:09 pm
Updated 11/30/16:
http://www.ashjournal.com/article/S1933-1711(16)30548-4/abstract
J Am Soc Hypertens. 2016 Oct 26.
Omega-3 fatty acids supplementation improves endothelial function and arterial stiffness in hypertensive patients with hypertriglyceridemia and high cardiovascular risk.
Association between hypertriglyceridemia and cardiovascular (CV) disease is still controversial. The purpose of this study was to compare omega-3 and ciprofibrate effects on the vascular structure and function in low and high CV risk hypertensive patients with hypertriglyceridemia. Twenty-nine adults with triglycerides 150-499 mg/dL were divided into low (<7.5%) and high (≥7.5%) CV risk, randomized to receive omega-3 fatty acids 1800 mg/d or ciprofibrate 100 mg/d for 12 weeks. Treatment was switched after 8-week washout. Clinical evaluation and vascular tests were assessed at baseline and after intervention. Peripheral (131 ± 3 to 125 ± 3 mm Hg, P < .05) and aortic (124 ± 3 to 118 ± 2 mg/dL, P < .05) systolic blood pressure were decreased by ciprofibrate in low-risk patients. In high-risk patients, pulse wave velocity was reduced (10.4 ± 0.4 to 9.4 ± 0.3 m/s, P < .05) and flow-mediated dilation was increased (11.1 ± 1.6 to 13.5 ± 1.2%, P < .05) by omega-3. In conclusion, omega-3 improved arterial stiffness and endothelial function, pointing out the beneficial effect of this therapy on vascular aging, in high-risk patients. Be well! JP
February 14th, 2017 at 12:12 am
Updated 02/13/17:
https://www.ncbi.nlm.nih.gov/pubmed/28189073
Environ Res. 2017 Feb 8;155:49-59.
Lower levels of Persistent Organic Pollutants, metals and the marine omega 3-fatty acid DHA in farmed compared to wild Atlantic salmon (Salmo salar).
Contaminants and fatty acid levels in farmed- versus wild Atlantic salmon have been a hot topic of debate in terms of food safety. The present study determined dioxins (polychlorinated dibenzo-p-dioxin and dibenzofuran), polychlorinated biphenyls (PCBs), polybrominated diphenyl ethers (PBDEs), organochlorine pesticides (OCPs), metals and fatty acids in wild and farmed Atlantic salmon. Contaminant levels of dioxins, PCBs, OCPs (DDT, dieldrin, lindane, chlordane, Mirex, and toxaphene), and mercury were higher in wild salmon than in farmed salmon, as were the concentrations of the essential elements selenium, copper, zinc and iron, and the marine omega-3 fatty acid docosahexaenoic acid (DHA). PBDE, endosulfan, pentachlorobenzene, hexachlorobenzene, cadmium and lead levels were low and comparable in both wild and farmed fish, and there was no significant difference in the marine omega-3 fatty acid eicosapentaenoic acid (EPA) concentration. The total fat content was significantly higher in farmed than wild salmon due to a higher content of both saturated and monounsaturated fatty acids, as well as a higher content of omega-6 fatty acids. The omega-3 to omega-6 fatty acid ratio was considerably lower in farmed than wild salmon due to the high level of omega-6 fatty acids. Contaminant concentrations in Atlantic salmon were well below maximum levels applicable in the European Union. Atlantic salmon, both farmed and wild, is a good source of EPA and DHA with a 200g portion per week contributing 3.2g or 2.8g respectively, being almost twice the intake considered adequate for adults by the European Food Safety Authority (i.e. 250mg/day or 1.75g/week).
Be well!
JP
June 25th, 2017 at 12:47 pm
Updated 06/25/17:
https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/high-intake-of-fatty-fish-but-not-of-lean-fish-improved-postprandial-glucose-regulation-and-increased-the-n3-pufa-content-in-the-leucocyte-membrane-in-healthy-overweight-adults-a-randomised-trial/46A086F341B075496C5042E9AE3B79E3
Br J Nutr. 2017 Jun 13:1-11.
High intake of fatty fish, but not of lean fish, improved postprandial glucose regulation and increased the n-3 PUFA content in the leucocyte membrane in healthy overweight adults: a randomised trial
The prevalence of type 2 diabetes (T2D) is low in populations with a high fish intake; however prospective studies with fish intake have shown positive, negative or no association between fish intake and the risk for T2D. The aim of this study was to investigate the effects of high intake of lean or fatty fish on glucose tolerance, leucocyte membrane fatty acid composition and leucocyte function in overweight/obese adults. In this randomised clinical trial, sixty-eight healthy overweight/obese participants consumed 750 g/week of either lean or fatty fish as dinners, or were instructed to continue their normal eating habits but to avoid fish intake (control group), for 8 weeks. Energy and macronutrient intake and physical activity were not changed within the groups during the study period. High intake of fatty fish, but not of lean fish, significantly improved glucose regulation 120 min postprandially (P=0·012), but did not affect fasting glucose concentration. A smaller increase in fasting to 120 min postprandial insulin C-peptide concentration was seen after fatty fish intake (P=0·012). Lean fish increased the DHA content in leucocyte membranes (P=0·010), and fatty fish increased the total content of n-3 PUFA (P=0·00016) and reduced the content of n-6 PUFA (P=0·00057) in leucocyte membranes. Lean and fatty fish intake did not affect phagocytosis of bacteria ex vivo. The findings suggest that high intake of fatty fish, but not of lean fish, beneficially affected postprandial glucose regulation in overweight/obese adults, and may therefore prevent or delay the development of T2D in this population.
Be well!
JP