Salt Sensitivity
May 11, 2011 Written by JP [Font too small?]There’s nothing like a controversial study to stir up the hornet’s nest that is modern medicine. If you think politics is contentious, just try going up against decades worth of health care policy and theories. That’s exactly what a small group of researchers from the University of Lueven, Belgium and the Journal of the American Medical Association (JAMA) did recently.

The current edition of JAMA includes a publication entitled, “Fatal and Nonfatal Outcomes, Incidence of Hypertension, and Blood Pressure Changes in Relation to Urinary Sodium Excretion”. The publication’s findings fly in the face of conventional wisdom that a higher intake of sodium is associated with greater cardiovascular disease (CVD) risk and mortality. The study itself involved 3,681 healthy adults that were followed on average for about 8 years. Urinary sodium levels, an indicator of sodium consumption, were measured at the start of the examination. Cardiovascular related deaths were then compared to 24 hour sodium excretion levels in the participants. The unexpected results indicate that those who excreted less sodium demonstrated a higher risk of CVD mortality. In terms of percentages, 4.1% of the lowest tertile of sodium excretion died due to CVD, 1.9% in the medium excretion group and only .8% in the those consuming the highest amount of sodium. And if that wasn’t enough of a shock, another study appearing in the March 2011 issue of Diabetes Care reports that, “In patients with type 2 diabetes, lower 24-hour urinary sodium excretion was paradoxically associated with increased all-cause and cardiovascular mortality”. Such findings add weight to a recent critical review of the current dietary guidelines which questioned the value of recommending sodium restriction for the population at large. (1,2,3)
To nobody’s surprise, the attention grabbing salt study has been met with criticism from experts on both sides of the salt debate. Dr. Ralph L. Sacco who heads up the American Heart Association, wryly remarked that “We need to take this article with a large grain of salt”. In an interview with WebMD, Dr. Sacco commented that 24-hour urinary excretion rates are subject to wide variations and could easily be misconstrued. Dr. Richard Feinman, professor of cell biology at SUNY Downstate Medical Center, took exception to the design of the trial itself. “Why not just plot the number of deaths vs. sodium excretion and time or something similar? Then everybody could see what kind of numbers and what kind of variation we are talking about.” It should be noted that Dr. Feinman was one of the co-authors of the critical review I alluded to in the previous paragraph, “In the Face of Contradictory Evidence: Report of the Dietary Guidelines for Americans Committee”. (4)
When reviewing the case against high sodium intake, several recent publications specifically come to mind. The February 2010 issue of the New England Journal of Medicine used a computer model to estimate the impact of reducing dietary salt intake by 3 grams per day in the United States. According to estimates, this simple strategy would lead to a projected yearly decline in coronary heart disease cases of between 60,000 to 120,000, heart attacks by 54,000 to 99,000 and strokes by 32,000 to 66,000. What’s more, the authors theorized that the health care savings involved could be as high as $24 billion a year. Much of the postulated benefits are based on the general expectation that lowering sodium consumption would result in a meaningful drop in blood pressure. Proponents of sodium restriction also draw attention to various population studies that have found an association between higher sodium intake and an increased risk of cardiovascular disease, ischemic stroke and even gastric cancer. (5,6,7,8,9,10,11,12,13,14)
Not everyone agrees that such epidemiological data should be applied as a matter of public policy. Once again, I turned to Dr. Feinman for a dissenting point of view: “You can’t treat a population. You can only treat people. My understanding is that even within hypertension where some people are helped by salt reduction, it is only some, some fraction of that population. So why treat everybody?”
Here’s one of the reasons why sodium is so often in the crosshairs of nutritional authorities. Numerous inquiries dating back to 1957 indicate that sodium consumption is well above the level required to sustain good health. Other minerals such as calcium, magnesium and potassium are frequently lacking. But sodium is uniformly found in excess in the average 21st century diet. Where is all this sodium coming from? A fair share makes its way into the food supply via processed foods. A study appearing in the March 2011 edition of the American Journal of Clinical Nutrition determined that only about 23% of daily sodium intake in England is in the form of table salt. The remainder comes from refined foods that tend to be heavily salted. This disproportionate shift in sodium intake puts modern man at odds with the traditional, nutrient dense diets of our ancestors. A scientific paper from 2006 examined the interaction and relationship between potassium and sodium in “Stone Age” and modern diets. The determination was that modern diets are frequently deficient in potassium and excessive in sodium. The authors from the University of California at San Francisco concluded that “the electrolytic mix of the modern diet is profoundly mismatched to its processing machinery” (ie the human body). (15,16,17,18,19,20,21,22)
Potassium Consumption Reduces Salt-Sensitivity
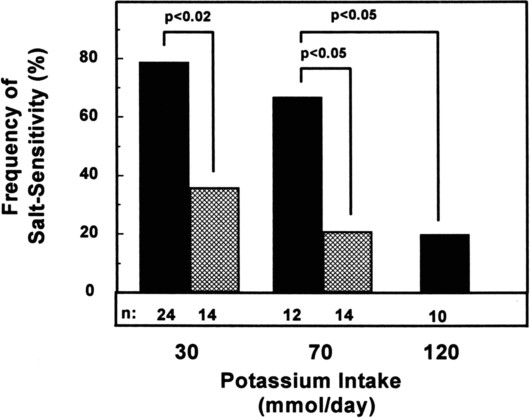
Source: J Am Coll Nutr June 2006 vol. 25 no. suppl 3 262S-270S (link)
The proportion of sodium to other nutrients isn’t the only problem some scientists are concerned about. Combining sodium with certain common food elements may also influence the way this mineral affects the body. Many refined meals and snacks are loaded with a form of sugar known as fructose. The interplay between fructose and sodium may be an important factor in the sodium/blood pressure connection. Animal and human studies suggest that dietary fructose enhances sodium absorption “in the small intestines and kidney tubules, resulting in a state of salt overload and thus causing hypertension”. In practical terms, this may mean that adding some table salt to a fillet of salmon could have a much lesser impact on blood pressure than a seemingly innocuous salad topped with a salty-sweet dressing. (23,24,25)
Here’s my personal perspective and some supporting evidence for it. Apart from population based data, some scientific interventions indicate that high salt meals: a) negatively impact post-prandial circulation as assessed by flow mediated dilatation and; b) raise blood pressure and pulse wave velocity, a measure of vascular function. On the other hand, adopting a low salt diet isn’t a panacea for cardiovascular and other diseases. Controlled studies have attempted and failed to show that lower sodium intake successfully: a) decreases coagulation; b) lowers inflammation or; c) modulates heart rate variability. There’s even some evidence that suggests that a low salt diet increases the likelihood of insulin resistance in healthy adults. (26,27,28,29,30,31)
In our household, we use two different types of salt. I season with a special form of sea salt that is naturally rich in potassium. Each serving provides 331 mg of potassium and 118 mg of sodium. Mrs. Healthy Fellow uses a separate sea salt with a sodium count of about 400 mg per serving. Why the difference? My wife prefers the taste of traditional sea salt in most dishes. I opt for the low sodium salt because several, well designed studies report that potassium rich salt substitutes may benefit arterial function and blood pressure. This works out well for the two of us as evidenced by consistently healthy blood pressure readings. What’s right for you? That’s for you and your health care team to determine. In closing, I’ll give the final word to Dr. Richard Feinman: “If we are going to make recommendations, they should be based on results that are unambiguous. These studies with low hazard ratios do not exclude the null hypothesis which is: salt consumption as regulated by individual taste and experience has no general detrimental effect on health. Some, but not all, individuals with hypertension may benefit from salt reduction.” (32,33,34,35,36)
Be well!
JP
Tags: High Blood Pressure, Potassium, Salt
Posted in Food and Drink, Heart Health, Nutrition

May 11th, 2011 at 5:36 pm
Comment and question for you, JP.
I eliminated soda pop from my diet as a way to curb my sodium intake. As you mentioned, I was told by my doctor that sodium may be partially at fault for my high blood pressure. Even if it’s not the case, I’m finding that I’m saving more money by not purchasing 80-100 ozs of pop a day. Heh.
Question: I know that iodine is added to salt in order to make sure people don’t get iodine-deficient ailments like gout. Since you’re using sea salt, are you getting iodine via another method?
May 11th, 2011 at 6:06 pm
Chris,
I take a daily multivitamin/mineral which provides 100% of the daily requirement of iodine. I also pick up some additional iodine via my diet from foods such as fish, nori and yogurt.
http://www.nlm.nih.gov/medlineplus/ency/article/002421.htm
https://www.healthyfellow.com/650/savory-sweet-nori-chips-recipe/
Be well!
JP
May 17th, 2011 at 11:49 am
My family uses Himalayan Crystal Salt. We found it to be the healthiest for us. According to our research natural crystal salt contains all the elements of which the human body is comprised.
Of course when we eat out or at family and friends we know they all cook with table salt or sea salt.
JP, what do you know about natural crystal salt?
May 17th, 2011 at 12:17 pm
Kelly,
What I like to do is to get an idea about just how much of the other minerals (besides sodium) these natural salts contain. Typically speaking, when I see their nutritional breakdown … they tend to only contain very small amounts of the other essential minerals. That’s why I’m hesitant to depend on most sources of salt for my nutritional needs.
Some specially formulated salts do provide a meaningful amount of potassium and sometimes magnesium. However they tend to be the exceptions to the rule, in my experience.
Be well!
JP
May 17th, 2011 at 1:08 pm
Thanks for the info. I will need to look at amounts in the natural crystal salt as compared to that of sea salt.
Cheers
June 1st, 2015 at 6:59 pm
Update 06/01/15:
http://archpedi.jamanetwork.com/article.aspx?articleid=2272973
JAMA Pediatr. 2015 Apr 27.
Longitudinal Effects of Dietary Sodium and Potassium on Blood Pressure in Adolescent Girls.
Importance: Identification of risk factors early in life for the development of high blood pressure is critical to the prevention of cardiovascular disease.
Objective: To study prospectively the effect of dietary sodium, potassium, and the potassium to sodium ratio on adolescent blood pressure.
Design, Setting, and Participants: The National Heart, Lung, and Blood Institute’s Growth and Health Study is a prospective cohort study with sites in Richmond, California; Cincinnati, Ohio; and Washington, DC. Participants included 2185 black and white girls initially aged 9 to 10 years with complete data for early-adolescent to midadolescent diet and blood pressure who were followed up for 10 years. The first examination visits were from March 1987 through February 1988 and follow-up continued until February 1999. Longitudinal mixed models and analysis of covariance models were used to assess the effect of dietary sodium, potassium, and the potassium to sodium ratio on systolic and diastolic blood pressures throughout adolescence and after 10 years of follow-up, adjusting for race, height, activity, television/video time, energy intake, and other dietary factors.
Exposures: Mean dietary sodium and potassium intakes and the mean potassium to sodium ratio in individuals aged 9 to 17 years. To eliminate potential confounding by energy intake, energy-adjusted sodium and potassium residuals were estimated.
Main Outcomes and Measures: Mean systolic and diastolic blood pressures throughout adolescence and at the end of follow-up (individuals aged 17-21 years).
Results: Sodium intakes were classified as less than 2500 mg/d (19.4% of participants), 2500 mg/d to less than 3000 mg/d (29.5%), 3000 mg/d to less than 4000 mg/d (41.4%), and 4000 mg/d or more (9.7%). Potassium intakes ranged from less than 1800 mg/d (36.0% of participants) to 1800 mg/d to less than 2100 mg/d (26.2%), 2100 mg/d to less than 2400 mg/d (18.8%), and 2400 mg/d or more (19.0%). There was no evidence that higher sodium intakes (3000 to <4000 mg/d and ≥4000 mg/d vs <2500 mg/d) had an adverse effect on adolescent blood pressure and longitudinal mixed models showed that those consuming 3500 mg/d or more had generally lower diastolic blood pressures compared with individuals consuming less than 2500 mg/d (P = .18). However, higher potassium intakes were inversely associated with blood pressure change throughout adolescence (P < .001 for systolic and diastolic) and at the end of follow-up (P = .02 and P = .05 for systolic and diastolic, respectively). While the potassium to sodium ratio was also inversely associated with systolic blood pressure (P = .04), these effects were generally weaker compared with effects for potassium alone. Conclusions and Relevance: In this study of adolescent girls, consumption of 3500 mg/d of sodium or more had no adverse effect on blood pressure. The beneficial effects of dietary potassium on both systolic and diastolic blood pressures suggest that consuming more potassium-rich foods during childhood may help suppress the adolescent increase in blood pressure. Be well! JP
April 6th, 2016 at 1:14 am
Updated 04/05/16:
http://jn.nutrition.org/content/146/4/838.abstract
J Nutr. 2016 Apr;146(4):838-45.
Salt Promotes Passive Overconsumption of Dietary Fat in Humans.
BACKGROUND: Excess fat consumption has been linked to the development of obesity. Fat and salt are a common and appetitive combination in food; however, the effect of either on food intake is unclear. Fat taste sensitivity has been negatively associated with dietary fat intake, but how fat taste sensitivity influences the intake of fat within a meal has, to our knowledge, not yet been investigated.
OBJECTIVES: Our objectives were, first, to investigate the effects of both fat and salt on ad libitum food intake and, second, to investigate the effects of fat taste sensitivity on satiation responses to fat and whether this was affected by salt.
METHODS: Forty-eight healthy adults [16 men and 32 women, aged 18-54 y, body mass index (kg/m(2)): 17.8-34.4] were recruited and their fat taste sensitivity was measured by determination of the detection threshold of oleic acid (18:1n-6). In a randomized 2 × 2 crossover design, participants attended 4 lunchtime sessions after a standardized breakfast. Meals consisted of elbow macaroni (56%) with sauce (44%); sauces were manipulated to be1) low-fat (0.02% fat, wt:wt)/low-salt (0.06% NaCl, wt:wt),2) low-fat/high-salt (0.5% NaCl, wt:wt),3) high-fat (34% fat, wt:/wt)/low-salt, or4) high-fat/high-salt. Ad libitum intake (primary outcome) and eating rate, pleasantness, and subjective ratings of hunger and fullness (secondary outcomes) were measured.
RESULTS: Salt increased food and energy intakes by 11%, independent of fat concentration (P= 0.022). There was no effect of fat on food intake (P= 0.6), but high-fat meals increased energy intake by 60% (P< 0.001). A sex × fat interaction was found (P= 0.006), with women consuming 15% less by weight of the high-fat meals than the low-fat meals. Fat taste sensitivity was negatively associated with the intake of high-fat meals but only in the presence of low salt (fat taste × salt interaction on delta intake of high-fat - low-fat meals;P= 0.012). CONCLUSIONS: The results suggest that salt promotes passive overconsumption of energy in adults and that salt may override fat-mediated satiation in individuals who are sensitive to the taste of fat. Be well! JP