Vitamin D and Dementia
March 28, 2012 Written by JP [Font too small?]Part of my responsibility as a medical researcher and natural health consultant is to present breaking information that your doctors may not be aware of and/or ready to share with you. Mainstream medicine is notorious for not advocating certain important health practices until they’re widely accepted by the institutions that govern it. On the other hand, holistic practitioners often veer to the opposite end of the spectrum and assign too much importance to theories that are only backed by preliminary evidence. Today’s blog features an evidence-based snapshot of a trend I’ve been seeing over the past few years. I believe the data contained herein will eventually be accepted by the alternative and conventional medical camps. But, you don’t have to wait until the Journal of the American Medical Association or some other pillar of modern medicine gives its seal of approval to enact the forthcoming research.
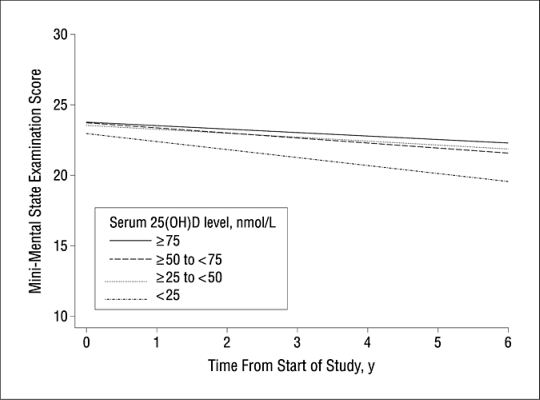
Current reviews inform us that as few as 15% of the senior population meets the criteria for adequate Vitamin D status as measured by serum 25-hydroxyvitamin D or 25(OH)D values. The first thing that may come to mind when hearing this are the consequences relating to osteopenia and osteoporosis risk in this growing population. However, the affects of suboptimal Vitamin D are now believed to be a modifiable risk factor in another predominant health condition impacting the elderly: dementia. Recent population studies from various countries point to a significantly greater risk of age-related, cognitive decline and dysfunction in older men and women with low Vitamin D status (<50 nmol/L). In addition, some evidence also draws a connection between objective changes in brain tissue such as increased brain lesions in seniors with hypovitaminosis D – a term used to describe a deficiency in this essential hormone/nutrient.
In fairness, I must say that not all allopathic institutions are passively observing the data involving Vitamin D and dementia. Drug manufacturers are actually quite interested in the possibility that inadequate D levels may increase the risk and symptoms associated with Alzheimer’s disease (AD) and other forms of dementia. Currently, there is a trial underway that is examining the effects of a combination of a medication (memantine) used to treat AD and an active form of Vitamin D (cholecalciferol or D3). The folks involved with drug development are keenly aware of published trials pointing to Vitamin D’s neuroprotective potential via multiple mechanisms including a reduction in inflammation, oxidative stress and the promotion of key substances in the brain such as nerve growth factor. All of this evidence, while preliminary, suggests good cause to have Vitamin D status tested in all adults and safely manipulated via supplementation when needed. There’s no good reason to wait for proof positive when the upsides are many and downsides aren’t expected.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Vitamin D in the Elderly: 5 Points to Remember … (link)
Study 2 – Vitamin D, Cognitive Dysfunction and Dementia in Older Adults … (link)
Study 3 – Vitamin D Insufficiency and Mild Cognitive Impairment: Cross- … (link)
Study 4 – Serum Vitamin D Deficiency as a Predictor of Incident Non-Alzheimer … (link)
Study 5 – Vitamin D and Cognitive Impairment in the Elderly U.S. Population … (link)
Study 6 – Vitamin D and Executive Function: A Preliminary Report … (link)
Study 7 – Vitamin D and Brain Imaging in the Elderly: Should we Expect Some … (link)
Study 8 – Possibility of a New Anti-Alzheimer’s Disease Pharmaceutical … (link)
Study 9 – Immunopathogenesis of Neurodegenerative Diseases: Current … (link)
Study 10 – The Beneficial Role of Vitamin D in Alzheimer’s Disease … (link)
Higher Vitamin D Levels May Slow Cognitive Decline
Source: Arch Intern Med. 2010;170(13):1135-1141. (link)
Tags: Alzheimer's, Dementia, Vitamin D
Posted in Alternative Therapies, Memory, Nutritional Supplements


March 28th, 2012 at 9:12 pm
My elderly mother’s mind is definitely better since I’ve taken over as her main caregiver. I give her 10,000iu D3/day, plus curcumin and the usual gamut of vitamins, fish/krill oil,etc. Taking her off Lipitor helped her more than anything.
This goes against standard altmed practice but she’s now taking a one week preemptive monthly round of doxycycline to prevent bronchitis. She was having to be hospitalized every 6 to 8 weeks previously. Now she’s gone 4 or 5 months without a bronchitis attack.
Believe me I was hesitant to try monthly antibiotics and I went through several hundred$ trying various natural remedies to no avail.
March 29th, 2012 at 1:10 am
Thanks for sharing that, Iggy. I’m happy to hear that your mom is feeling better.
It seems that statin drugs commonly affect cognition in many users. I know many physicians adore this class of medication, but I certainly have many reservations about them.
Almost anything that keeps you out the hospital is a good trade-off. Ironically, hospitals can be very dangerous places – even when you’re not there for invasive procedures. And, the risks only go up for senior patients.
Your experience also highlights that importance of judiciously using medications when they’re the best option available. A world without medications wouldn’t be as rosy as some suspect. Having access to the best of both worlds (allopathic and alterative) is vital, IMO.
Be well!
JP
March 29th, 2012 at 4:39 am
10,000 iu? isnt that a bit too much?btw jp could you recommend me a good daily dosage of vitamin d pls? because with all those recommended intakes that come from anyone, i got a bit confused. thx a lot!the funny part is that all those vitamin d deficiencies could be solved easily by taking a 15 minute afternoon walk ^^
March 29th, 2012 at 10:53 am
Question: Have you seen many intervention trials showing that adding D3 helps slow or reverse disease progression? Most of what I’ve seen only shows correlation between low 25(OH)D levels and increased disease — which raises questions of why the D is low in the first place (beyond sun phobias and sunscreen).
Great work always, JP!
—Dr. O
March 29th, 2012 at 1:04 pm
Hi, Geos.
10,000 IUs *can* be too high, but only blood testing can determine that for certain. In my experience, most people require less. However, some people benefit from even higher dosages – at least in the short term.
Also, not everyone synthesizes adequate Vitamin D concentrations via sun exposure. Time and time again, scientists are surprised to find sub-optimal D levels in those living in sunny climates. That’s why testing is so important. It’s inexpensive, widely available and worth it, IMO.
If testing isn’t possible, a (very) general dosage worth considering is 2,000 IUs/day – preferably taken with the largest meal of the day.
Be well!
JP
March 29th, 2012 at 1:19 pm
Before supplementing with D you really should test for it, because it can vary greatly as to what people need. (Same can be said about any vitamins people supp. with)
March 29th, 2012 at 1:22 pm
Hi, Orna.
There haven’t been many published intervention trials as of yet. However, a few are in the works. To my mind, maintaining optimal D levels prior to the onset of dementia will likely be the key to success. I suspect that using D as a treatment for dementia will be a more hit-and-miss proposition. As always, prevention is preferable to trying to reverse established damage.
Here’s a link to a study that’s currently recruiting and not mentioned in my column:
http://clinicaltrials.gov/ct2/show/NCT01315704?term=vitamin+d+dementia&rank=2
Another study with disappointing results. But, Vitamin D2 was used in conjunction with insulin in this case.
http://www.ncbi.nlm.nih.gov/pubmed/21694461
Be well!
JP
March 29th, 2012 at 2:47 pm
Hi Rob.
I agree about the importance of 25(OH)D testing. If asked, many physicians are willing to order it for their patients. My parents and others have found this to be true. Otherwise, it can be ordered/paid for by patients directly at a reasonable cost – usually $50 or so.
Be well!
JP
April 7th, 2015 at 7:39 pm
Update: Low Vit D status linked to cognitive impairment and dementia risk in seniors …
http://onlinelibrary.wiley.com/doi/10.1111/cen.12733/abstract
Clin Endocrinol (Oxf). 2015 Feb 2.
Serum 25-hydroxyvitamin D level and the risk of mild cognitive impairment and dementia: the Korean Longitudinal Study on Health and Aging (KLoSHA).
OBJECTIVE: The association of low vitamin D status with mild cognitive impairment (MCI), a preclinical condition that can lead to dementia, has not yet been fully explored. Our aim was to investigate the association between vitamin D status and the future risk of MCI and dementia in older adults.
DESIGN, SETTING AND PARTICIPANTS: We conducted a population-based prospective study as a part of the Korean Longitudinal Study on Health and Aging. Four hundred and twelve elderly participants who completed evaluations of cognitive function and metabolic parameters in 2005-2006 and 2010-2011 were analysed.
MAJOR OUTCOME MEASURE: The rate of development of MCI or dementia during the study period was compared according to baseline vitamin D status. Binary logistic regression analysis was performed to investigate any independent association between vitamin D status and the risks of MCI or dementia.
RESULTS: Among 405 subjects that remained after excluding seven demented subjects at baseline, 338 subjects remained unchanged or improved in their diagnosis for cognitive function during the study period, whereas 67 subjects showed progression to MCI or dementia. When analyzing 236 subjects whose baseline mini-mental state examination (MMSE) scores were <27, severe vitamin D deficiency at baseline, defined as <25 nmol/l, was independently associated with the progression of cognitive impairment. Among 297 subjects who were normal at baseline, 50 acquired MCI and 247 remained normal. Severe vitamin D deficiency was also independently associated with the development of MCI when analyzing 145 subjects whose baseline MMSE scores were <27.
CONCLUSION: Severe vitamin D deficiency was independently associated with the future risk of MCI as well as dementia, especially in older adults whose baseline MMSE scores had decreased only modestly.
Be well!
JP
July 10th, 2015 at 10:01 am
Update 07/10/15:
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=9795973&fulltextType=RA&fileId=S0007114515001749
Br J Nutr. 2015 Jun 23:1-10. [Epub ahead of print]
Association between mild cognitive impairment and dementia and undernutrition among elderly people in Central Africa: some results from the EPIDEMCA (Epidemiology of Dementia in Central Africa) programme.
Several studies in Western countries have shown an association between cognitive disorders and low BMI or weight loss in elderly people. However, few data are available in Africa. We analysed the association between cognitive disorders and undernutrition among elderly people in Central Africa. A cross-sectional, multicentre, population-based study using a two-phase design was carried out in subjects aged 65 years and above in the Central African Republic (CAR) and the Republic of Congo (ROC). All subjects were interviewed using the Community Screening Interview for Dementia, and those with low performance were clinically assessed by a neurologist and underwent further psychometrical tests. Diagnostic and Statistical Manual-IV and Petersen’s criteria were required for the diagnoses of dementia and mild cognitive impairment (MCI), respectively. Undernutrition was evaluated using mid-upper arm circumference (MUAC) < 24 cm, BMI < 18·5 kg/m2 and arm muscular circumference (AMC) < 5th percentile. Multivariate binary logistic regression models were used to estimate the associations. In CAR, MCI was associated with MUAC < 24 cm (OR 0·7, 95 % CI 0·4, 1·0) and dementia with BMI < 18·5 kg/m2 (OR 2·3, 95 % CI 1·6, 3·1), AMC < 5th percentile (OR 2·3, 95 % CI 1·1, 4·6) and MUAC < 24 cm (OR 1·8, 95 % CI 1·4, 2·4). In ROC, both MCI and dementia were associated with all markers of undernutrition, but only AMC < 5th percentile was significantly associated with MCI (OR 3·1, 95 % CI 1·9, 4·8). In conclusion, cognitive disorders were associated with undernutrition. However, further studies are needed to elucidate the relationship between MCI and undernutrition in CAR. Be well! JP
August 3rd, 2015 at 7:57 pm
Updated 08/03/15:
http://www.nutritionj.com/content/14/1/76
Nutr J. 2015 Aug 1;14(1):76.
Vitamin D deficiency is associated with increased risk of Alzheimer’s disease and dementia: evidence from meta-analysis.
BACKGROUND: In recent years, the associations between vitamin D status and Alzheimer’s disease (AD) and dementia have gained increasing interests. The present meta-analysis was designed to estimate the association between vitamin D deficiency and risk of developing AD and dementia.
METHODS: A literature search conducted until February 2015 identified 10 study populations, which were included in the meta-analysis. Pooled risk ratios (RRs) and 95 % confidence interval (CI) were calculated with a random-effect model using Stata software package.
RESULTS: Results of our meta-analysis showed that subjects with deficient vitamin D status (25(OH)D level < 50 nmol/L) were at increased risk of developing AD by 21 % compared with those possessing 25(OH)D level > 50 nmol/L. Similar analysis also found a significantly increased dementia risk in vitamin D deficient subjects. There is no evidence for significant heterogeneity among the included studies.
CONCLUSION: Available data indicates that lower vitamin D status may be associated with increased risk of developing AD and dementia. More studies are needed to further confirm the associations and to evaluate the beneficial effects of vitamin D supplementation in preventing AD and dementia.
Be well!
JP
September 16th, 2015 at 3:50 pm
Updated 09/16/15:
http://medicalxpress.com/news/2015-09-vitamin-d-cognitive-decline-older.html
In a study published Sept. 15 in the Journal of the American Medical Association-Neurology, Joshua Miller, professor of nutritional sciences at the Rutgers School of Environmental and Biological Sciences, found that people with low levels of vitamin D experienced rates of cognitive decline at a much faster pace than people with adequate vitamin D status.
“There were some people in the study who had low vitamin D who didn’t decline at all and some people with adequate vitamin D who declined quickly,” said Miller. “But on average, people with low vitamin D declined two to three times as fast as those with adequate vitamin D.”
Full Text of Study: http://archneur.jamanetwork.com/article.aspx?articleid=2436596
JAMA Neurol. 2015 Sep 14.
Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults.
Importance: Vitamin D (VitD) deficiency is associated with brain structural abnormalities, cognitive decline, and incident dementia.
Objective: To assess associations between Vit D status and trajectories of change in subdomains of cognitive function in a cohort of ethnically diverse older adults.
Design, Setting, and Participants: Longitudinal multiethnic cohort study of 382 participants in an outpatient clinic enrolled between February 2002 and August 2010 with baseline assessment and yearly follow-up visits. Serum 25-hydroxyvitamin D (25-OHD) was measured, with VitD status defined as the following: deficient, less than 12 ng/mL (to convert to nanomoles per liter, multiply by 2.496); insufficient, 12 to less than 20 ng/mL; adequate, 20 to less than 50 ng/mL; or high, 50 ng/mL or higher. Subdomains of cognitive function were assessed using the Spanish and English Neuropsychological Assessment Scales. Associations were evaluated between 25-OHD levels (as continuous and categorical [deficient, insufficient, or adequate]) and trajectories of cognitive decline.
Main Outcomes and Measures: Serum 25-OHD levels, cognitive function, and associations between 25-OHD levels and trajectories of cognitive decline.
Results: Participants (N = 382 at baseline) had a mean (SD) age of 75.5 (7.0) years; 61.8% were women; and 41.4% were white, 29.6% African American, 25.1% Hispanic, and 3.9% other race/ethnicity. Diagnosis at enrollment included 17.5% with dementia, 32.7% with mild cognitive impairment, and 49.5% cognitively normal. The mean (SD) 25-OHD level was 19.2 (11.7) ng/mL, with 26.2% of participants being VitD deficient and 35.1% insufficient. The mean (SD) 25-OHD levels were significantly lower for African American and Hispanic participants compared with white participants (17.9 [15.8] and 17.2 [8.4] vs 21.7 [10.0] ng/mL, respectively; P < .001 for both). The mean (SD) 25-OHD levels were similarly lower in the dementia group compared with the mild cognitive impairment and cognitively normal groups (16.2 [9.4] vs 20.0 [10.3] and 19.7 [13.1] ng/mL, respectively; P = .006). The mean (SD) follow-up was 4.8 (2.5) years. Rates of decline in episodic memory and executive function among VitD-deficient (episodic memory: β = -0.04 [SE = 0.02], P = .049; executive function: β = -0.05 [SE = 0.02], P = .01) and VitD-insufficient (episodic memory: β = -0.06 [SE = 0.02], P < .001; executive function: β = -0.04 [SE = 0.02], P = .008) participants were greater than those with adequate status after controlling for age, sex, education, ethnicity, body mass index, season of blood draw, vascular risk, and apolipoprotein E4 genotype. Vitamin D status was not significantly associated with decline in semantic memory or visuospatial ability. Exclusion of participants with dementia did not substantially affect the associations between VitD status and rates of cognitive decline. Conclusions and Relevance: Low VitD status was associated with accelerated decline in cognitive function domains in ethnically diverse older adults, including African American and Hispanic individuals who exhibited a high prevalence of VitD insufficiency or deficiency. It remains to be determined whether VitD supplementation slows cognitive decline. Be well! JP
September 28th, 2015 at 8:52 am
Updated 09/28/15:
https://www.dovepress.com/serum-25-hydroxyvitamin-d-predicts-cognitive-performance-in-adults-peer-reviewed-fulltext-article-NDT
Neuropsychiatric Disease and Treatment August 2015 Volume 2015:11
Background: Vitamin D is an endogenous hormone known to regulate calcium levels in the body and plays a role in cognitive performance. Studies have shown an association between vitamin D deficiency and cognitive impairment in older adults. Lebanon has a high 25-hydroxyvitamin D (25(OH)D) deficiency prevalence across all age groups.
Methods: In this cross-sectional study, we explored the cognitive performance and serum 25(OH)D levels using an electrochemoluminescent immunoassay in 254 older (>60 years) as well as younger (30–60 years) adults. Subjects’ characteristics, including age, years of education, wearing of veil, alcohol consumption, smoking, and physical exercise, were collected. Participants were screened for depression prior to cognitive screening using the Montreal Cognitive Assessment Arabic version. Visuospatial memory was tested using the Rey Complex Figure Test and Recognition Trial, and speed of processing was assessed using the Symbol Digit Modalities test.
Results: Pearson’s correlation and stepwise linear regression analyses showed that a low vitamin D level was associated with greater risk of cognitive impairment in older as well as younger adults.
Conclusion: These findings suggest that correction of vitamin D needs to be explored as an intervention to prevent cognitive impairment. Prospective longitudinal studies are needed to ascertain the effect of such interventions.
Be well!
JP
November 11th, 2015 at 6:18 pm
Updated 11/11/15:
http://link.springer.com/article/10.1007%2Fs12035-015-9516-4
Mol Neurobiol. 2015 Nov 9.
Dietary Patterns and Risk of Dementia: a Systematic Review and Meta-Analysis of Cohort Studies.
Dietary patterns and some dietary components have been linked with dementia. We therefore performed a meta-analysis of available studies to determine whether there is an association between diet and risk of dementia. We included eligible articles and estimated risk ratio (RR) with 95 % confidence intervals (95 % CIs). Finally, there were 43 trials that met the inclusion standard. Some food intake was related with decrease of dementia, such as unsaturated fatty acids (RR: 0.84, 95 % CI: [0.74-0.95], P = 0.006), antioxidants (RR: 0.87, 95 % CI: [0.77-0.98], P = 0.026), vitamin B (RR: 0.72, 95 % CI: [0.54-0.96], P = 0.026), and the Mediterranean diet (MeDi) (RR: 0.69, 95 % CI: [0.57-0.84], P < 0.001). Some material intakes were related with increase of dementia, such as aluminum (RR: 2.24, 95 % CI: [1.49-3.37], P < 0.001), smoking (RR: 1.43, 95 % CI: [1.15-1.77], P = 0.001), and low levels of vitamin D (RR: 1.52, 95 % CI: [1.17-1.98], P = 0.002). The effect of some materials needs further investigation, such as fish (RR: 0.79, 95 % CI: [0.59-1.06], P = 0.113), vegetables and fruits (RR: 0.46, 95 % CI: [0.16-1.32], P = 0.149), and alcohol (RR: 0.74, 95 % CI: [0.55- 1.01], P = 0.056). Thus, the MeDi and higher consumption of unsaturated fatty acids, antioxidants, and B vitamins decrease the risk of dementia while smoking and higher consumption of aluminum increase the risk of dementia. Low levels of vitamin D were associated with cognitive decline. The effect of fish, vegetables, fruits, and alcohol needs further investigation. The findings will be of great significance to guide people to prevent dementia. Be well! JP
May 13th, 2016 at 11:38 am
Updated 05/13/16:
http://www.ncbi.nlm.nih.gov/pubmed/27168052
J Am Med Dir Assoc. 2016 May 7. pii: S1525-8610(16)30061-5.
Comparing the Effects of Cognitive Stimulation, Reminiscence, and Aroma-Massage on Agitation and Depressive Mood in People With Dementia.
PURPOSE: Cognitive stimulation therapy (CST), reminiscence therapy (RT), and aroma-massage therapy (AT) are believed to be beneficial for people with dementia (PwD). However, the comparing effects of these interventions have not been reported in previous studies. The purpose of this research was thus to compare the effects of these 3 interventions on alleviating agitation and depressive mood in PwD.
DESIGN: A cohort study with pre- and post-tests was conducted.
METHODS: A total of 102 PwD from 10 long-term care facilities were allocated to RT (n = 43), CST (n = 29), or AT (n = 29) groups. The participants received the interventions once a week for 8 to 10 consecutive weeks. The participants were evaluated using the Chinese version of the Cohen-Mansfield Agitation Inventory and the Cornell Scale for Depression in Dementia before and shortly after the intervention. One-way ANOVA and ANCOVA were used to analyze the data.
RESULTS: Significant differences in the effects on agitation and depressive symptoms in PwD were found among the 3 interventions (P = .013 and P < .001, respectively). Post hoc analysis showed that AT was more effective than RT and CST in improving agitated behaviors (P = .006 and P < .001, respectively), and was also more effective than CST and RT in alleviating depressive symptoms (both P < .001). CONCLUSIONS: Our findings indicate that among the 3 alternative remedies, AT can be a more effective intervention than CST and RT with regard to alleviating the agitated behavior and depressive symptoms of PwD. Given that agitated behavior and depressive mood are common among institutionalized PwD, and staff working in long-term care facilities often lack knowledge and time to manage such behaviors, the findings of this study can contribute to future clinical practice in long-term care facilities. In addition, aroma-massage has the advantage of being an easy-to-learn intervention for staff working with PwD. Be well! JP
May 7th, 2017 at 4:09 pm
Updated 05/07/17:
https://www.ncbi.nlm.nih.gov/pubmed/28475473
Nutr Neurosci. 2017 May 5:1-9.
The effect of vitamin D supplement on the score and quality of sleep in 20-50 year-old people with sleep disorders compared with control group.
OBJECTIVES: Sleep quality may be directly related with vitamin D serum level. Some studies found that people with lower vitamin D serum level experienced a lower sleep quality. Consequently, this study aimed at determining the effect of vitamin D supplements on sleep score and quality in 20-50 year-old people with sleep disorders.
METHODS: This double blind, clinical trial was performed in November 2015-February 2016 on 89 people with sleep disorders based on Petersburg’s Sleep Index. Patient samples were divided randomly into two groups: intervention and placebo. At the end of the study, the data on 89 subjects (44 in intervention group and 45 people in placebo group) were examined. Intervention group received a 50 000-unit vitamin D supplement, one in a fortnight for 8 weeks. Meanwhile, placebo group received placebo. Before and after intervention, Petersburg’s Sleep Quality Questionnaire, International Physical Activity Questionnaire, general information questionnaire, sun exposure, vitamin D serum level and 3-day food record questionnaire were assessed and recorded for all participants. To analyze data, t-test, chi square, ANCOVA, U-Mann-Whitney and Wilcoxon statistical tests were used.
FINDINGS: Based on the results of the present study, at the end of the study sleep score (PSQI) reduced significantly in vitamin recipients as compared with placebo recipients (P < 0.05). This difference was significant even after modifying confounding variables (P < 0.05). CONCLUSION: This study shows that the use of vitamin D supplement improves sleep quality, reduces sleep latency, raises sleep duration and improves subjective sleep quality in people of 20-50 year-old with sleep disorder. Be well! JP
June 23rd, 2017 at 6:19 pm
Updated 06/23/17:
http://www.mdpi.com/2072-6643/9/7/647
Nutrients 2017, 9(7), 647
Vitamin D3 and 25-Hydroxyvitamin D3 Content of Retail White Fish and Eggs in Australia
Dietary vitamin D may compensate for inadequate sun exposure; however, there have been few investigations into the vitamin D content of Australian foods. We measured vitamin D3 and 25-hydroxyvitamin D3 (25(OH)D3) in four species of white fish (barramundi, basa, hoki and king dory), and chicken eggs (cage and free-range), purchased from five Australian cities. Samples included local, imported and wild-caught fish, and eggs of varying size from producers with a range of hen stocking densities. Raw and cooked samples were analysed using high performance liquid chromatography with photodiode array. Limits of reporting were 0.2 and 0.1 μg/100 g for vitamin D3 and 25(OH)D3, respectively. The vitamin D3 content of cooked white fish ranged from <0.1 to 2.3 μg/100 g, and the 25(OH)D3 content ranged from 0.3 to 0.7 μg/100 g. The vitamin D3 content of cooked cage eggs ranged from 0.4 to 0.8 μg/100 g, and the 25(OH)D3 content ranged from 0.4 to 1.2 μg/100 g. The vitamin D3 content of cooked free-range eggs ranged from 0.3 to 2.2 μg/100 g, and the 25(OH)D3 content ranged from 0.5 to 0.8 μg/100 g. If, as has been suggested, 25(OH)D3 has five times greater bioactivity than vitamin D3, one cooked serve (100 g) of white fish, and one cooked serve of cage or free-range eggs (120 g) may provide 50% or 100%, respectively, of the current guidelines for the adequate intake of vitamin D (5 µg) for Australians aged 1–50 years.
Be well!
JP