Fish Oil News for Women
March 5, 2013 Written by JP [Font too small?]Holistic practitioners pride themselves in treating individuals based on their unique needs and requirements. However, even when dealing with a holistic physician, it’s still important to make sure that you are indeed receiving personalized care. For instance, the effects of any given supplement may have slightly or significantly different effects based on age, gender and medical history. In practice, this could mean that one form of fish oil is better suited for pregnant women and another for those trying to improve exercise performance.
A slew of recent studies are helping to define how to best use omega-3 fatty acid supplements in female populations. Some of the latest findings reveal that: 1) Taking supplemental fish oil, but not plant-based omega-3s, such as chia seeds, assist with body fat and weight loss. In addition, “long chain polyunsaturated fatty acids” support physical performance which, in turn, promotes consistent exercise and healthier body composition. 2) Taking a minimum of 200 mg of DHA, a fatty acid found in fish oil, and a maximum of 600 mg daily reduces the risk of premature birth and very low birth weight. The use of pre and postnatal DHA has, likewise, been shown to benefit cardiovascular function (i.e. higher heart rate variability) and a healthier body mass index (BMI) in children followed up to the age of six. 3) Fish oil rich in DHA more effectively lowers platelet aggregation, a measure of “blood thinning”, than EPA rich fish oil. EPA is another prominent, long-chain fatty acid contained in fish and fish oil. 4) Supplemental fish oil should be considered a viable therapy for women with polycystic ovary syndrome (PCOS), “a common female endocrine disorder associated with several risk factors of type 2 diabetes and cardiovascular diseases”. A recent trial involving 64 women with PCOS found that 4 grams/day of fish oil, providing a total of 480 DHA and 720 EPA, improved various markers of cardiometabolic health including elevated insulin, high triglycerides, low adiponectin and HDL (“good”) cholesterol.
Finally, if you need one more reason to consider taking fish oil, do it for your skin. A study published in the March 2013 issue of the American Journal of Clinical Nutrition reports that fish oil supplementation prevents UV-related photoimmunosuppression. By protecting the skin against solar ultraviolet radiation, fish oil therapy may minimize the risk of skin cancer.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Prior Supplementation w/ Long Chain Omega-3 Polyunsaturated Fatty … (link)
Study 2 – The Impact of Supplemental N-3 Long Chain Polyunsaturated Fatty Acids … (link)
Study 3 – Chia Seed Supplementation and Disease Risk Factors in Overweight … (link)
Study 4 – Supplementation of Milled Chia Seeds Increases Plasma ALA and EPA … (link)
Study 5 – DHA Supplementation and Pregnancy Outcomes … (link)
Study 6 – Effects of Docosahexaenoic Acid Supplementation During Pregnancy … (link)
Study 7 – Does Docosahexaenoic Acid (DHA) Status in Pregnancy Have Any Impact … (link)
Study 8 – Eicosapentaenoic and Docosahexaenoic Acid Supplementation Reduces … (link)
Study 9 – Effects of Omega-3 Fatty Acids Supplementation on Serum Adiponectin … (link)
Study 10 – Randomized Controlled Trial of Oral Omega-3 PUFA in Solar-Simulated … (link)
Fish Oil Supplements May Increase Muscle Strength in Older Women
Source: Am J Clin Nutr February 2012 vol. 95 no. 2 428-436 (link)
Tags: Diabetes, PCOS, Skin Care
Posted in Heart Health, Nutritional Supplements, Women's Health


January 20th, 2015 at 12:17 am
The primary reason fish oil is a better source of omega-3 fatty acids is that plant sources of omega-3 (flax, canola and walnut oils, greens) must be converted to the “animal form”. This conversion is inefficient, about 10:1. That is, only 10% of the plant source omega-3’s are converted by the body to what our body uses directly, which is EPA and DHA. Since EPA and DHA are found in fish ready made, fish oil is a much more effective source for most people. However, vegetarians can still get the necessary omega-3’s from plant sources with regular consumption.
January 20th, 2015 at 2:07 pm
Hi, Harlan.
A quick note: Nowadays, there are also vegetarian sources of preformed EPA & DHA. They’re typically derived from algae. They’re a decent alternative for those who choose or must avoid fish.
Be well!
JP
July 20th, 2015 at 9:38 pm
Updated 07/20/15:
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=9860784&fileId=S0007114515001555
Br J Nutr. 2015 Jul;114(1):43-52.
Influence of fish oil supplementation and strength training on some functional aspects of immune cells in healthy elderly women.
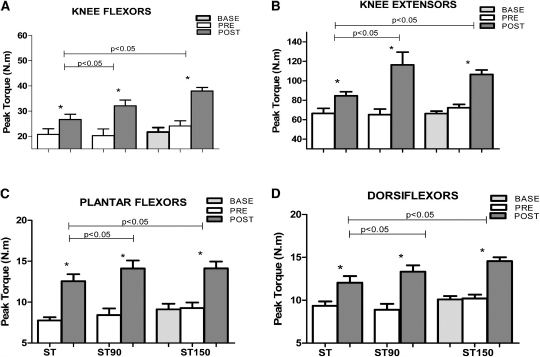
Immune function changes with ageing and is influenced by physical activity (strength training, ST) and diet (fish oil, FO). The present study investigated the effect of FO and ST on the immune system of elderly women. Forty-five women (64 (sd 1·4) years) were assigned to ST for 90 d (ST; n 15), ST plus 2 g/d FO for 90 d (ST90; n 15) or 2 g/d FO for 60 d followed by ST plus FO for 90 d (ST150; n 15). Training was performed three times per week, for 12 weeks. A number of innate (zymosan phagocytosis, lysosomal volume, superoxide anion, peroxide of hydrogen) and adaptive (cluster of differentiation 4 (CD4), CD8, TNF-α, interferon-γ (IFN-γ), IL-2, IL-6 and IL-10 produced by lymphocytes) immune parameters were assessed before supplementation (base), before (pre-) and after (post-) training. ST induced no immune changes. FO supplementation caused increased phagocytosis (48 %), lysosomal volume (100 %) and the production of superoxide anion (32 %) and H2O2 (70 %) in the ST90. Additional FO supplementation (ST150) caused no additive influence on the immune system, as ST150 and ST90 did not differ, but caused greater changes when compared to the ST (P< 0·05). FO increased CD4+ and CD8+ lymphocytes in the ST150, which remained unchanged when training was introduced. The combination of ST and FO reduced TNF-α in the ST150 from base to post-test. FO supplementation (ST150, base-pre) when combined with exercise (ST150, pre-post) increased IFN-γ, IL-2, IL-6 and IL-10 production. The immune parameters improved in response to FO supplementation; however, ST alone did not enhance the immune system. Be well! JP
July 20th, 2015 at 9:44 pm
Updated 07/20/15:
http://www.ncbi.nlm.nih.gov/pubmed/25882499
Public Health Nutr. 2015 Apr 17:1-8.
Fish and fish-liver oil consumption in adolescence and midlife and risk of CHD in older women.
OBJECTIVE: To study the association of fish and fish-liver oil consumption across the lifespan with CHD later in life among Icelandic women, with special emphasis on the effects of consumption in adolescence.
DESIGN: Prevalence association study. Logistic regression was used to estimate odds ratios and 95 % confidence intervals of CHD according to fish or fish-liver oil exposure. Models were adjusted for age, education, concurrent diet and other known risk factors.
SETTING: The study was nested within the AGES-Reykjavik Study, conducted in Reykjavik, Iceland.
SUBJECTS: Participants were 3326 women aged 66-96 years, with available information on CHD status at entry to the study and information on fish and fish-liver oil consumption during midlife and adolescence. Dietary habits were assessed retrospectively using a validated FFQ.
RESULTS: CHD was identified in 234 (7·9 %) women. Compared with women with no intake of fish-liver oil in adolescence or midlife, women who consumed fish-liver oil at least three times weekly in adolescence or in midlife had a decreased risk of CHD (OR=0·62; 95 % CI 0·45, 0·85 and OR=0·68; 95 % CI 0·50, 0·94, respectively). No associations were observed between fish intake (>2 portions/week v. ≤2 portions/week) in adolescence or midlife and CHD in this population with high fish intake.
CONCLUSIONS: Fish-liver oil consumption, from early life, may reduce the risk of CHD in older women. Lifelong nutrition may be of importance in the prevention of CHD in older women.
Be well!
JP
July 20th, 2015 at 9:46 pm
Updated 07/20/15:
http://aje.oxfordjournals.org/content/181/9/691.abstract
Am J Epidemiol. 2015 May 1;181(9):691-705.
Associations of the Ratios of n-3 to n-6 Dietary Fatty Acids With Longitudinal Changes in Depressive Symptoms Among US Women.
In the present study, we examined longitudinal changes in self-reported depressive symptoms (and related domains) in relation to baseline intakes of n-3 fatty acids (absolute and relative to n-6 fatty acids). Sex-specific associations were evaluated in a prospective cohort of adults (n = 2,053) from Baltimore, Maryland, who were 30-64 years of age at baseline and were followed for a mean of 4.65 (standard deviation, 0.93) years (2004-2013). Using mean intakes of n-3 and n-6 fatty acids reported on two 24-hour dietary recalls, we estimated the ratios of n-3 to n-6 fatty acids for both highly unsaturated fatty acids (≥20 carbon atoms) (HUFAs) and polyunsaturated fatty acids (≥18 carbon atoms) (PUFAs). Outcomes included total and domain-specific scores on the 20-item Center for Epidemiologic Studies-Depression scale. Based on mixed-effects regression models, among women, both higher n-3 HUFA:n-6 PUFA and n-3 PUFA:n-6 PUFA ratios were associated with a slower rate of increase in total Center for Epidemiologic Studies-Depression scores over time. Higher n-3 HUFA:n-6 HUFA ratios were associated with slower increases in somatic complaints in men, whereas among women, higher n-3 HUFA:n-6 PUFA and n-3 PUFA:n-6 PUFA ratios were both linked to putative longitudinal improvement in positive affect over time. Among US adults, n-3:n-6 dietary fatty acid ratio was associated with longitudinal changes in depressive symptoms, with a higher ratio linked to a slower increase in depressive symptoms over time, particularly among women.
Be well!
JP
July 20th, 2015 at 9:48 pm
Updated 07/20/15:
http://ajcn.nutrition.org/content/101/4/824.abstract
Am J Clin Nutr. 2015 Apr;101(4):824-34.
Long-chain ω-3 fatty acid intake and endometrial cancer risk in the Women’s Health Initiative.
BACKGROUND: Inflammation may be important in endometrial cancer development. Long-chain ω-3 (n-3) polyunsaturated fatty acids (LCω-3PUFAs) may reduce inflammation and, therefore, reduce cancer risk. Because body mass is associated with both inflammation and endometrial cancer risk, it may modify the association of fat intake on risk.
OBJECTIVE: We examined whether intakes of LCω-3PUFAs were associated with endometrial cancer risk overall and stratified by body size and histologic subtype.
DESIGN: Women were n = 87,360 participants of the Women’s Health Initiative Observational Study and Clinical Trials who were aged 50-79 y, had an intact uterus, and completed a baseline food-frequency questionnaire. After 13 y of follow-up, n = 1253 incident invasive endometrial cancers were identified. Cox regression models were used to estimate HRs and 95% CIs for the association of intakes of individual ω-3 fatty acids and fish with endometrial cancer risk.
RESULTS: Intakes of individual LCω-3PUFAs were associated with 15-23% linear reductions in endometrial cancer risk. In women with body mass index (BMI; in kg/m(2)) <25, those in the upper compared with lowest quintiles of total LCω-3PUFA intake (sum of eicosapentaenoic, docosapentaenoic, and docosahexaenoic acids) had significantly reduced endometrial cancer risk (HR: 0.59; 95% CI: 0.40, 0.82; P-trend = 0.001), whereas there was little evidence of an association in overweight or obese women. The reduction in risk observed in normal-weight women was further specific to type I cancers.
CONCLUSIONS: Long-chain ω-3 intake was associated with reduced endometrial cancer risk only in normal-weight women. Additional studies that use biomarkers of ω-3 intake are needed to more accurately estimate their effects on endometrial cancer risk.
Be well!
JP
July 20th, 2015 at 9:49 pm
Updated 07/20/15:
http://onlinelibrary.wiley.com/doi/10.1002/oby.20966/abstract
Obesity (Silver Spring). 2015 Feb;23(2):313-21.
Effects of α-lipoic acid and eicosapentaenoic acid in overweight and obese women during weight loss.
OBJECTIVE: To evaluate the potential body weight-lowering effects of dietary supplementation with eicosapentaenoic acid (EPA) and α-lipoic acid separately or combined in healthy overweight/obese women following a hypocaloric diet.
METHODS: This is a short-term double-blind placebo-controlled study with parallel design that lasted 10 weeks. Of the randomized participants, 97 women received the allocated treatment [Control, EPA (1.3 g/d), α-lipoic acid (0.3 g/d), and EPA+α-lipoic acid (1.3 g/d+0.3 g/d)], and 77 volunteers completed the study. All groups followed an energy-restricted diet of 30% less than total energy expenditure. Body weight, anthropometric measurements, body composition, resting energy expenditure, blood pressure, serum glucose, and insulin and lipid profile, as well as leptin and ghrelin levels, were assessed at baseline and after nutritional intervention.
RESULTS: Body weight loss was significantly higher (P<0.05) in those groups supplemented with α-lipoic acid. EPA supplementation significantly attenuated (P<0.001) the decrease in leptin levels that occurs during weight loss. Body weight loss improved lipid and glucose metabolism parameters but without significant differences between groups.
CONCLUSIONS: The intervention suggests that α-lipoic acid supplementation alone or in combination with EPA may help to promote body weight loss in healthy overweight/obese women following energy-restricted diets.
Be well!
JP