Peripheral Artery Disease Alternatives
January 29, 2015 Written by JP [Font too small?]Lack of adequate blood flow can affect many areas of the body. When insufficient circulation targets the legs, it’s frequently caused by a condition known as PAD or peripheral artery disease. In PAD, hardening of leg arteries and accumulation of plaque lead to a narrowing effect and diminished blood flow. Subsequently those with PAD often suffer from uncomfortable symptoms, including leg cramping, numbness and pain – especially during periods of physical activity. More importantly, a PAD diagnosis may increase the risk of heart attack, stroke and poor wound healing in the lower region of the body. Fortunately, emerging research indicates that certain foods and exercises can limit PAD symptoms and some of the associated risks.
Here are ten strategies to naturally address PAD. You can incorporate one or more into your daily routine. In all likelihood, the more you do, the better results you’ll find. However, please keep in mind that peripheral artery disease is a serious medical matter, much like cardiovascular disease. If you suspect you may have undiagnosed PAD, please consult your doctor to establish a confirmed diagnosis.
1. A February 2014 study in the British Journal of Nutrition reports that eating 37 grams daily of dark chocolate enhances vasodilation (widening of blood vessels) and reduces arterial stiffness.
2. The October 2013 edition of Atherosclerosis found that consuming half a cup of cooked beans, chickpeas, lentils and peas improved circulation to the limbs as verified by an increase in the ankle-brachial index of 26 PAD patients.
3. A 2012 trial revealed that ongoing intake of tomato paste (70 grams/daily, yielding 33.3 mg of lycopene) boosted a key measure of circulation known as flow mediated dilatation or FMD.
4. In 2013, researchers determined that higher levels of omega-3 fats were associated with lower levels of inflammation in a group of PAD patients. Peripheral artery disease is characterized by a pro-inflammatory state. Eating more cold water fish and other sources of omega-3 fats may help to moderate excess inflammation.
5. A study appearing in the December 2010 issue of the Journal of the American College of Nutrition informs that plant-based sources of omega-3 fats (alpha-linolenic acid) may also be of value. Specifically, flaxseed oil, walnuts and walnut oil demonstrated beneficial effects on blood pressure, flow mediated vasodilation and peripheral resistance.
6. In June 2014, a group of Japanese scientists discovered that the addition of curry to a high carbohydrate meal prevents detrimental changes in post-meal circulation.
7. A primary challenge for many PAD patients is the inability to exercise as long they’d like without cramping or pain. Drinking a few glasses of beetroot juice daily has been scientifically shown to lengthen “peak walking time” and reduce claudication pain. It is hypothesized that this effect is attributable to an increase in peripheral tissue oxygenation.
8. There’s a lot of debate about how much salt truly impacts vascular function. A study in the May 2011 edition of the American Journal of Clinical Nutrition doesn’t mince words. The authors conclude that a high salt meal (HSM), “which reflects the typical amount of salt consumed in a commonly eaten meal, can significantly suppress brachial artery FMD within 30 minutes”.
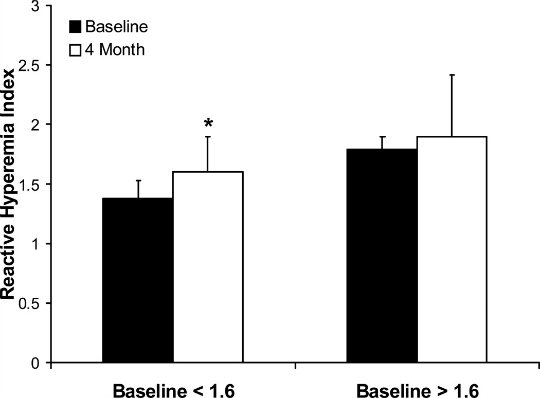
9. A single session of resistance exercise increases vasodilation and reduces reactive hyperemia – blocked or impaired blood flow – so say a group of Brazilian researchers in the January 2015 issue of Applied Physiology, Nutrition, and Metabolism.
10. A 2013 experiment documented in the Journal of the American Medical Association, describes how a simple, home-based walking program is also capable of improving walking endurance and speed in PAD patients. This is particularly good news for those who may not have access to a gym or supervised training.
You may have noticed that several of the remedies in today’s column also appeared in my recent piece entitled, “Better Blood Pressure”. Often times, natural cardiovascular remedies tend to provide far reaching benefits. For instance, you may take something to specifically improve circulation and find anti-inflammatory, blood pressure and/or cholesterol-lowering benefits. This is what I commonly refer to as a “side benefit”, as opposed to the side effects that are all too commonly found when using conventional medications.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Effects of Dark Chocolate & Cocoa Consumption on Endothelial Function … (link)
Study 2 – Daily Non-Soy Legume Consumption Reverses Vascular Impairment … (link)
Study 3 – Tomato Paste Supplementation Improves Endothelial Dynamics … (link)
Study 4 – Association Between N-3 Polyunsaturated Fatty Acid Content of Red … (link)
Study 5 – Effects of Diets High in Walnuts and Flax Oil on Hemodynamic Responses … (link)
Study 6 – A Single Consumption of Curry Improved Postprandial Endothelial … (link)
Study 7 – Dietary Nitrate Supplementation Enhances Exercise Performance … (link)
Study 8 – Endothelial Function is Impaired After a High-Salt Meal in Healthy … (link)
Study 9 – A Session of Resistance Exercise Increases Vasodilation in Intermittent … (link)
Study 10 – Home-Based Walking Exercise Intervention in Peripheral Artery … (link)
High-Polyphenol Olive Oil Improves Vascular Function
Source: Eur J Nutr. 2013 Apr;52(3):1223-31. (link)
Tags: Beans, Curry, Lycopene, Salt
Posted in Alternative Therapies, Exercise, Nutrition


February 1st, 2015 at 11:18 pm
Hi JP,
Very valuable article!
I will start implementing your recommendations and report back in a month the progress in my legs pain and energy.
Thank you!
Paul
February 2nd, 2015 at 11:48 am
Thank you, Paul! I look forward to hearing about your experience!
Be well!
JP
February 2nd, 2015 at 4:48 pm
Update: Today, I received an invaluable email from a thoughtful reader suggesting that some of the terms I mentioned in this column may benefit from added description. This is a valid point and one that I grapple with in each new piece I write. I strive to find the right balance between too much medical or scientific explanation and too little. Therefore, below I’ll paste the accurate and more detailed definitions of several terms mentioned in the column above. I hope they help deepen your understanding of this important topic.
—
“Perhaps some clarifications could be considered so the reader may be more satisfied:
In item #2 you mentioned “ankle brachial index” which is the ratio of the blood pressure in the lower legs to the blood pressure in the arms.
In #3 you touch upon flow mediated dilatation or FMD. This is a research tool used to compare the diameter of the brachial artery diameter measured through ultrasound between the moment it is under the pressure of a cuff and after the pressure is released.
Item #7 references peak walking distance or the walking time at which ambulation cannot continue due to maximal leg pain, thereby forcing the discontinuation of a treadmill test.”
—
I appreciate your contribution, friend. 🙂
Be well!
JP
February 10th, 2015 at 5:17 pm
Update: Nut intake appears to lower PAD risk …
http://www.sciencedirect.com/science/article/pii/S0091743514004964
Prev Med. 2014 Dec 19;72C:15-18.
Greater frequency of nut consumption is associated with lower prevalence of peripheral arterial disease.
Nut consumption has been associated with lower risk of coronary heart disease and all-cause mortality. The association between nut intake and peripheral arterial disease (PAD) is uncertain.
OBJECTIVE:
We sought to investigate the association between nut consumption and presence of prevalent PAD in a large cross-sectional sample.
METHODS:
Self-referred participants at >20,000 US sites who completed a medical and lifestyle questionnaire were evaluated by screening ankle brachial indices for PAD. Multivariable logistic regression analysis was used to estimate odds of PAD in different nut consumption categories.
RESULTS:
Among 3,312,403 individuals, mean age was 63.6±10.6years and 62.8% were female. There were 219,527 cases of PAD. After multivariable adjustment there was an inverse association of nut intake with PAD. Compared to subjects with consumption of nuts
February 20th, 2015 at 2:25 pm
Update: Vitamin K2 (MK-7) improves arterial stiffness in older women …
http://www.ncbi.nlm.nih.gov/pubmed/25694037
Thromb Haemost. 2015 Feb 19;113(5).
Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women: double-blind randomised clinical trial.
Observational data suggest a link between menaquinone (MK, vitamin K2) intake and cardiovascular (CV) health. However, MK intervention trials with vascular endpoints are lacking. We investigated long-term effects of MK-7 (180 µg MenaQ7/day) supplementation on arterial stiffness in a double-blind, placebo-controlled trial. Healthy postmenopausal women (n=244) received either placebo (n=124) or MK-7 (n=120) for three years. Indices of local carotid stiffness (intima-media thickness IMT, Diameter end-diastole and Distension) were measured by echotracking. Regional aortic stiffness (carotid-femoral and carotid-radial Pulse Wave Velocity, cfPWV and crPWV, respectively) was measured using mechanotransducers. Circulating desphospho-uncarboxylated matrix Gla-protein (dp-ucMGP) as well as acute phase markers Interleukin-6 (IL-6), high-sensitive C-reactive protein (hsCRP), tumour necrosis factor-α (TNF-α) and markers for endothelial dysfunction Vascular Cell Adhesion Molecule (VCAM), E-selectin, and Advanced Glycation Endproducts (AGEs) were measured. At baseline dp-ucMGP was associated with IMT, Diameter, cfPWV and with the mean z-scores of acute phase markers (APMscore) and of markers for endothelial dysfunction (EDFscore). After three year MK-7 supplementation cfPWV and the Stiffness Index β significantly decreased in the total group, whereas distension, compliance, distensibility, Young’s Modulus, and the local carotid PWV (cPWV) improved in women having a baseline Stiffness Index β above the median of 10.8. MK-7 decreased dp-ucMGP by 50 % compared to placebo, but did not influence the markers for acute phase and endothelial dysfunction. In conclusion, long-term use of MK-7 supplements improves arterial stiffness in healthy postmenopausal women, especially in women having a high arterial stiffness.
Be well!
JP
February 20th, 2015 at 9:21 pm
Update: Flax seeds lower LDL (“bad”) cholesterol in PAD patients …
http://jn.nutrition.org/content/early/2015/02/18/jn.114.204594.abstract
J Nutr. 2015 Feb 18. pii: jn.114.204594.
Dietary Flaxseed Independently Lowers Circulating Cholesterol and Lowers It beyond the Effects of Cholesterol-Lowering Medications Alone in Patients with Peripheral Artery Disease.
BACKGROUND: Dietary flaxseed lowers cholesterol in healthy subjects with mild biomarkers of cardiovascular disease (CVD).
OBJECTIVE: The aim was to investigate the effects of dietary flaxseed on plasma cholesterol in a patient population with clinically significant CVD and in those administered cholesterol-lowering medications (CLMs), primarily statins.
METHODS: This double-blinded, randomized, placebo-controlled trial examined the effects of a diet supplemented for 12 mo with foods that contained either 30 g of milled flaxseed [milled flaxseed treatment (FX) group; n = 58] or 30 g of whole wheat [placebo (PL) group; n = 52] in a patient population with peripheral artery disease (PAD). Plasma lipids were measured at 0, 1, 6, and 12 mo.
RESULTS: Dietary flaxseed in PAD patients resulted in a 15% reduction in circulating LDL cholesterol as early as 1 mo into the trial (P = 0.05). The concentration in the FX group (2.1 ± 0.10 mmol/L) tended to be less than in the PL group (2.5 ± 0.2 mmol/L) at 6 mo (P = 0.12), but not at 12 mo (P = 0.33). Total cholesterol also tended to be lower in the FX group than in the PL group at 1 mo (11%, P = 0.05) and 6 mo (11%, P = 0.07), but not at 12 mo (P = 0.24). In a subgroup of patients taking flaxseed and CLM (n = 36), LDL-cholesterol concentrations were lowered by 8.5% ± 3.0% compared with baseline after 12 mo. This differed from the PL + CLM subgroup (n = 26), which increased by 3.0% ± 4.4% (P = 0.030) to a final concentration of 2.2 ± 0.1 mmol/L.Conclusions: Milled flaxseed lowers total and LDL cholesterol in patients with PAD and has additional LDL-cholesterol-lowering capabilities when used in conjunction with CLMs.
Be well!
JP
March 2nd, 2015 at 4:06 pm
Update: Chickpea flour helps to moderate increases in post-meal blood sugar …
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=9446828&fileId=S0007114514003031
Br J Nutr. 2014 Dec;112(12):1966-73.
The acute effect of commercially available pulse powders on postprandial glycaemic response in healthy young men.
Whole pulses (beans, peas, chickpeas and lentils) elicit low postprandial blood glucose (BG) responses in adults; however, their consumption in North America is low. One potential strategy to increase the dietary intake of pulses is the utilisation of commercial pulse powders in food products; however, it is unclear whether they retain the biological benefits observed with whole pulses. Therefore, the present study examined the effects of commercially prepared pulse powders on BG response before and after a subsequent meal in healthy young men. Overall, three randomised, within-subject experiments were conducted. In each experiment, participants received whole, puréed and powdered pulses (navy beans in Expt 1; lentils in Expt 2; chickpeas in Expt 3) and whole-wheat flour as the control. All treatments were controlled for available carbohydrate content. A fixed-energy pizza meal (50·2 kJ/kg body weight) was provided at 120 min. BG concentration was measured before (0-120 min) and after (140-200 min) the pizza meal. BG concentration peaked at 30 min in all experiments, and pulse forms did not predict their effect on BG response. Compared with the whole-wheat flour control, navy bean treatments lowered peak BG concentrations (Expt 1, P< 0.05), but not the mean BG concentration over 120 min. The mean BG concentration was lower for all lentil (Expt 2, P= 0.008) and chickpea (Expt 3, P= 0.002) treatments over 120 min. Processing pulses to powdered form does not eliminate the benefits of whole pulses on BG response, lending support to the use of pulse powders as value-added food ingredients to moderate postprandial glycaemic response. Be well! JP
June 26th, 2015 at 2:08 pm
Update 06/26/15:
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0107003
PLoS One. 2014 Sep 5;9(9):e107003.
Importance of fatty acid compositions in patients with peripheral arterial disease.
OBJECTIVE: Importance of fatty acid components and imbalances has emerged in coronary heart disease. In this study, we analyzed fatty acids and ankle-brachial index (ABI) in a Japanese cohort.
METHODS: Peripheral arterial disease (PAD) was diagnosed in 101 patients by ABI ≤0.90 and/or by angiography. Traditional cardiovascular risk factors and components of serum fatty acids were examined in all patients (mean age 73.2±0.9 years; 81 males), and compared with those in 373 age- and sex-matched control subjects with no evidence of PAD.
RESULTS: The presence of PAD (mean ABI: 0.71±0.02) was independently associated with low levels of gamma-linolenic acid (GLA) (OR: 0.90; 95% CI: 0.85-0.96; P = 0.002), eicosapentaenoic acid∶arachidonic acid (EPA∶AA) ratio (OR: 0.38; 95% CI: 0.17-0.86; P = 0.021), and estimated glomerular filtration rate (OR: 0.97; 95% CI: 0.96-0.98; P<0.0001), and with a high hemoglobin A1c level (OR: 1.34; 95% CI: 1.06-1.69; P = 0.013). Individuals with lower levels of GLA (≤7.95 µg/mL) and a lower EPA∶AA ratio (≤0.55) had the lowest ABI (0.96±0.02, N = 90), while the highest ABI (1.12±0.01, N = 78) was observed in individuals with higher values of both GLA and EPA∶AA ratio (P<0.0001).
CONCLUSION: A low level of GLA and a low EPA∶AA ratio are independently associated with the presence of PAD. Specific fatty acid abnormalities and imbalances could lead to new strategies for risk stratification and prevention in PAD patients.
Be well!
JP
July 13th, 2015 at 6:37 pm
Update 07/13/15:
http://www.ncbi.nlm.nih.gov/pubmed/26129736
Vasc Med. 2015 Jun 30.
Analysis of nutritional habits and intake of polyunsaturated fatty acids in veterans with peripheral arterial disease.
Inadequate nutrient intake may contribute to the development and progression of peripheral arterial disease (PAD). This study’s aim was to assess intake of essential fatty acids and nutrients among veterans with PAD. All 88 subjects had ankle-brachial indices of <0.9 and claudication. A validated food frequency questionnaire evaluated dietary intake, and values were compared to guidelines established by the American Heart Association (AHA) and American College of Cardiology (ACC), as well as the AHA/ACC endorsed Dietary Approaches to Stop Hypertension (DASH) eating plan. The mean age was 69 ± 8 years. Compared to the AHA/ACC guidelines, subjects with PAD had an inadequate intake of long-chain polyunsaturated fatty acids (n-3 PUFA; 59% consumed >1 gram daily). Our subjects with PAD had an increased intake of cholesterol (31% met the cut-off established in the DASH plan), total fat (5%) and sodium (53%). They had an inadequate intake of magnesium (3%), calcium (5%), and soluble fiber (3%). Dietary potassium intake met the recommended guidelines. In our subjects with PAD, intake of critical nutrients deviated substantially from the recommended amounts. Further prospective studies should evaluate whether PAD patients experience clinical benefit if diets are modified to meet the AHA/ACC recommendations.
Be well!
JP
December 30th, 2015 at 12:21 am
Updated 12/29/15:
https://www.thieme-connect.de/DOI/DOI?10.1055/s-0035-1556060
Int J Angiol. 2015 Dec;24(4):268-74.
A Clinical Comparison of Pycnogenol, Antistax, and Stocking in Chronic
Venous Insufficiency.
This 8-week registry study was a comparative evaluation of Pycnogenol
(French Maritime Pine Bark extract; Horphag Research, Geneva) and
Antistax (grape leaf extract [GLE, Boehringer Ingelheim, Germany]) in
controlling symptoms of chronic venous insufficiency (CVI). “Standard
management” for CVI is compression; a group of comparable subjects was
monitored to evaluate the effects of stockings. The registry included
183 patients (166 completing). Supplementation with Antistax (two
tablets of 360 mg/d) or Pycnogenol (100 mg/d) was used. The groups
were comparable for age, symptoms, venous incompetence, and
microcirculation (with increased capillary filtration and skin flux)
at inclusion. At 8 weeks, the rate of swelling (p < 0.05) and skin flux decreased toward normal values; changes were more important with Pycnogenol (p < 0.05). Transcutaneous Po 2 was increased more with Pycnogenol (p < 0.05). Ankle circumference was decreased more (p < 0.05) with Pycnogenol. An analog scale quantified symptoms. At 8 weeks, pain and edema were decreased with Pycnogenol and elastic compression (p < 0.05) with prevalence for Pycnogenol (p < 0.05). Edema with Pycnogenol was decreased by 40%. Induration was reduced only in the Pycnogenol group (p < 0.05) with minimal variations in the other groups. Tolerability and compliance were optimal. Elastic compression was correctly used by 80% of the patients indicating that it may be more difficult to use, particularly in warmer days. Costs for Pycnogenol were lower (96; 3.3 Euros) in comparison with the other groups (132;1.4 Euros for GLE and 149; 2.2 Euros for compression). Be well! JP
March 11th, 2016 at 2:19 am
Updated 03/10/16:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4759860/
J Int Soc Sports Nutr. 2016 Feb 19;13:6.
Oral L-citrulline supplementation enhances cycling time trial performance in healthy trained men: Double-blind randomized placebo-controlled 2-way crossover study.
BACKGROUND: Many human studies report that nitric oxide (NO) improves sport performance. This is because NO is a potential modulator of blood flow, muscle energy metabolism, and mitochondrial respiration during exercise. L-Citrulline is an amino acid present in the body and is a potent endogenous precursor of L-arginine, which is a substrate for NO synthase. Here, we investigated the effect of oral L-citrulline supplementation on cycling time trial performance in humans.
METHODS: A double-blind randomized placebo-controlled 2-way crossover study was employed. Twenty-two trained males consumed 2.4 g/day of L-citrulline or placebo orally for 7 days. On Day 8 they took 2.4 g of L-citrulline or placebo 1 h before a 4-km cycling time trial. Time taken to complete the 4 km cycle, along with power output/VO2 ratio (PO/VO2), plasma nitrite and nitrate (NOx) and amino acid levels, and visual analog scale (VAS) scores, was evaluated.
RESULTS: L-Citrulline supplementation significantly increased plasma L-arginine levels and reduced completion time by 1.5 % (p < 0.05) compared with placebo. Moreover, L-citrulline significantly improved subjective feelings of muscle fatigue and concentration immediately after exercise. CONCLUSIONS: Oral L-citrulline supplementation reduced the time take to complete a cycle ergometer exercise trial. Be well! JP
August 7th, 2016 at 6:59 pm
Updated 08/07/16:
http://www.ncbi.nlm.nih.gov/pubmed/27494446
Atherosclerosis. 2016 Jul 25;252:15-20.
The relationship between vitamin K and peripheral arterial disease.
BACKGROUND AND AIMS: A high dietary intake of vitamin K1 (phylloquinone) and vitamin K2 (menaquinones) is thought to decrease cardiovascular disease risk by reducing vascular calcification. The objective of this study is to explore if there is a relationship between phylloquinone and menaquinones intake and risk of PAD.
METHODS: We investigated the association between intake of phylloquinone and menaquinones with PAD in a prospective cohort with 36,629 participants. Occurrence of PAD was obtained by linkage to national registries. Baseline intake of phylloquinone and menaquinones was estimated using a validated food-frequency questionnaire. Multivariate Cox regression was used to estimate adjusted hazard ratio’s for the association.
RESULTS: During 12.1 years (standard deviation 2.1 years) of follow-up, 489 incident cases of PAD were documented. Menaquinones intake was associated with a reduced risk of PAD with a hazard ratio (HR) of 0.71, 95% CI; 0.53-0.95 for the highest versus lowest quartile. A stronger association was observed (p interaction 0.0001) in participants with hypertension (HRQ4 versus Q1 0.59; 95% CI 0.39-0.87) or diabetes (HRQ4 versus Q1 0.56; 95% CI 0.18-1.91), though confidence intervals were wide in the small (n = 530) diabetes stratum. Phylloquinone intake was not associated with PAD risk.
CONCLUSIONS: High intake of menaquinones was associated with a reduced risk of PAD, at least in hypertensive participants. High intake of phylloquinone was not associated with a reduced risk of PAD.
Be well!
JP
September 2nd, 2016 at 3:57 pm
Updated 09/02/16:
http://cpr.sagepub.com/content/early/2016/08/22/2047487316665231.abstract
Eur J Prev Cardiol. 2016 Aug 22.
Supervised exercise training in peripheral arterial disease increases vascular shear stress and profunda femoral artery diameter.
BACKGROUND: Arteriogenesis is promoted by flow- and pressure-related forces such as tangential wall stress and laminar shear stress. Exercise training (ET) is known to promote arteriogenesis in peripheral arterial disease (PAD) patients. It remains unclear whether supervised ET (SET) promotes arteriogenesis more efficiently than non-SET (nSET).
METHODS AND RESULTS: Forty PAD patients participated in a SET or nSET training programme (n = 20 each) and were compared to 20 healthy individuals without any history of cardiovascular events. Femoral artery diameter, flow and velocity were measured by ultrasound. Tangential wall stress and laminar shear stress were calculated for femoral arteries. Follow-up was performed after a mean of 7.65 ± 1.62 months. At follow-up, only the SET group showed a significant increase in lumen diameter of the profunda femoral artery (p = 0.03), accompanied by an increase of tangential wall stress (p = 0.002). Laminar shear stress decreased, but remained higher for the SET group compared to controls (p < 0.01). Individual changes in walking distance were higher for SET patients (p = 0.01) than nSET patients (p = 0.07). Profunda femoral lumen diameter and tangential wall stress correlated directly with walking distance (r = 0.446; p < 0.001), as well as with each other (r = 0.743; p < 0.0001). CONCLUSIONS: Our results indicate that SET promotes arteriogenesis more efficiently than nSET. Femoral lumen diameter and flow might help with the monitoring of ET efficiency and potential arteriogenesis. Be well! JP
February 17th, 2017 at 11:33 pm
02/17/17:
https://www.ncbi.nlm.nih.gov/pubmed/28206732
Int Angiol. 2017 Feb 15.
Clinical efficacy and safety of a new once-daily 1000 mg suspension versus twice-daily 500 mg tablets of micronized purified flavonoid fraction in patients with symptomatic chronic venous disorders: a randomized controlled trial.
BACKGROUND: Chronic venous disorders (CVD) is estimated to affect 30% to 50% of women and 10% to 30% of men. The most widely prescribed treatment for CVD worldwide is micronized purified flavonoid fraction 500 mg (MPFF). The aim of this clinical trial was to develop a new once daily 1000 mg oral suspension of MPFF.
METHODS: In an international, randomized, double-blind, parallel-group study, symptomatic individuals classified CEAP C0s to C4s were randomized in either treatment arm and treated for 8 weeks. Lower limb symptoms (discomfort, pain and heaviness) were assessed using visual analog scales (VAS), and QOL was measured with CIVIQ-20.
RESULTS: 1139 patients were included in the study. Both MPFF treatments regimen were well tolerated and associated with a significant reduction in lower limb symptoms. A non-inferiority of MPFF 1000 mg oral suspension once daily compared to MPFF 500 mg tablet twice daily (P<.0001) was found for lower limb discomfort (-3.33 cm for MPFF 1000 mg and -3.37 cm for MPFF 500 mg), leg pain (-3.27 cm for MPFF 1000 mg and -3.31 cm for MPFF 500 mg) and leg heaviness (-3.41 cm for MPFF 1000 mg and -3.46 cm for MPFF 500 mg). The patients' QOL was improved by about 20 points on the CIVIQ scale in both groups (19.33 points for MPFF 1000 mg and 20.28 points for MPFF 500 mg). CONCLUSIONS: MPFF 1000 mg oral suspension and MPFF 500 mg tablets treatments were associated with similar reductions in lower limb symptoms and QOL improvement. The new once daily MPFF1000 mg oral suspension has a similar safety profile to two tablets of MPFF 500 mg, with the advantage of one daily intake, potentially associated with improved patient adherence and easier CVD management. Be well! JP
March 15th, 2017 at 1:42 pm
Updated 03/15/17:
http://www.jvascsurg.org/article/S0741-5214(17)30081-2/abstract
J Vasc Surg. 2017 Mar 9.
Calf raise exercise increases walking performance in patients with intermittent claudication.
BACKGROUND: Symptoms of intermittent claudication (IC) are improved by exercise. The improvement might be secondary to increased blood perfusion or increased muscle mitochondrial capacity. Ischemia followed by reperfusion, also named preconditioning, is known to stimulate the mitochondria. We focused on a calf raise exercise inducing preconditioning in the calf muscle of patients with IC. We hypothesized that 8 weeks of this exercise would increase walking performance and mitochondrial capacity without a change in blood flow.
METHODS: Patients with IC were randomized to either a calf raise exercise group (n = 14) or a traditional walking exercise group (n = 15). The calf raise group was instructed to perform a specific type of calf raise exercise three times a day. The walking group was instructed to walk near the pain threshold at least 30 minutes three times a week. Both interventions lasted 8 weeks and were not supervised. Measurements of walking performance, mitochondrial capacity, peak oxygen uptake, peripheral hemodynamics, and health-related quality of life were obtained on each patient before and after the intervention period. Adherence was measured by a training diary, and an activity monitor was used.
RESULTS: The calf raise group improved pain-free walking distance by 44 meters (P = .04) and maximal walking distance by 99 meters (P = .047). Furthermore, claudication onset time increased by 123 seconds (P = .02), and peak walking time increased by 104 seconds (P = .01). The calf raise group increased the enzyme citrate synthase activity, which is a biomarker of mitochondrial volume-density in the muscle tissue (P = .02). The walking group did not increase any of these variables. Maximal blood flow, peak oxygen uptake, and mitochondrial respiration did not change in any group. The calf raise group experienced less disease anxiety (P < .01). Adherence to the instruction of exercise was 100% in the calf raise group and 80% in the walking group. The calf raise group maintained physical activity. A reduction in activity (P < .01) was found in the walking group. CONCLUSIONS: Calf raise exercise improves walking performance and increases mitochondrial volume-density in the gastrocnemius muscle without increasing blood flow in patients with IC. Be well! JP
January 3rd, 2018 at 10:14 pm
Updated 1/3/18:
https://www.jstage.jst.go.jp/article/ihj/58/4/58_16-373/_pdf/-char/en
Int Heart J. 2017 Aug 3;58(4):577-583.
Resveratrol Ameliorates Arterial Stiffness Assessed by Cardio-Ankle Vascular Index in Patients With Type 2 Diabetes Mellitus.
Resveratrol has been reported to have potent anti-atherosclerotic effects in animal studies. However, there are few interventional studies in human patients with atherosclerogenic diseases. The cardio-ankle vascular index (CAVI) reflects arterial stiffness and is a clinical surrogate marker of atherosclerosis. The aim of the present study was to investigate the effect of resveratrol on arterial stiffness assessed by CAVI in patients with type 2 diabetes mellitus (T2DM).In this double-blind, randomized, placebo-controlled study, 50 patients with T2DM received supplement of a 100mg resveratrol tablet (total resveratrol: oligo-stilbene 27.97 mg/100 mg/day) or placebo daily for 12 weeks. CAVI was assessed at baseline and the end of study. Body weight (BW), blood pressure (BP), glucose and lipid metabolic parameters, and diacron-reactive oxygen metabolites (d-ROMs; an oxidative stress marker) were also measured.Resveratrol supplementation decreased systolic BP (-5.5 ± 13.0 mmHg), d-ROMs (-25.6 ± 41.8 U.CARR), and CAVI (-0.4 ± 0.7) significantly (P < 0.05) and decreased BW (-0.8 ± 2.1 kg, P = 0.083) and body mass index (-0.5 ± 0.8 kg/m2, P = 0.092) slightly compared to baseline, while there were no significant changes in the placebo group. Decreases in CAVI and d-ROMs were significantly greater in the resveratrol group than in the placebo group. Multivariate logistic regression analysis identified resveratrol supplementation as an independent predictor for a CAVI decrease of more than 0.5.In conclusion, 12-week resveratrol supplementation may improve arterial stiffness and reduce oxidative stress in patients with T2DM. Resveratrol may be beneficial in preventing the development of atherosclerosis induced by diabetes. However, a large-scale cohort study is required to validate the present findings. Be well! JP
January 21st, 2019 at 8:08 pm
Updated 01/21/19:
https://www.atherosclerosis-journal.com/article/S0021-9150(18)31524-7/fulltext
Atherosclerosis. 2018 Dec 20.
Serum magnesium and the prevalence of peripheral artery disease: The Atherosclerosis Risk in Communities (ARIC) study.
BACKGROUND AND AIMS: Peripheral arterial disease (PAD) is a clinical manifestation of extracoronary atherosclerosis. Many risk factors are involved in the process of PAD, but the association between serum magnesium (Mg) and PAD is not clear. Our study aimed to investigate whether serum Mg is associated with PAD incidence.
METHODS: A total of 13,826 participants (aged 40-64 years) in the Atherosclerosis Risk in Communities (ARIC) study (1987-1989) without prior PAD were included in the final analysis. Serum Mg levels were measured at visits 1 and 2. PAD was defined as an ankle brachial index less than 0.9, or hospitalization with a PAD diagnosis. Cox regression was used to calculate hazard ratios (HRs) for incidence of PAD and serum Mg.
RESULTS: During a median follow-up of 24.4 years, 1364 (48.4% female) PAD events were observed. After multiple adjustment, participants in the lowest (≤1.4 mEq/L) category of serum Mg compared with the highest (≥1.8 mEq/L) ones were at higher PAD risk (HR: 1.3; 95% confidence interval (CI): 1.06-1.58) (p value = 0.004). The HRs for PAD in 1.5, 1.6 and 1.7 mEq/L of serum Mg were 1.29 (95% CI: 1.08-1.54), 1.05 (95% CI: 0.89-1.24), and 1.0 (95% CI: 0.85-1.18), respectively.
CONCLUSIONS: Low serum Mg was independently associated with an increased prevalence of PAD in the large population-based study; further studies are needed to confirm our findings.
Be well!
JP
April 8th, 2019 at 2:58 pm
Updated 04/08/19:
https://www.ncbi.nlm.nih.gov/pubmed/30940301
Pharmazie. 2019 Apr 1;74(4):193-200.
Therapeutic approach to chronic venous insufficiency – clinical benefits of red-vine-leaf-extract AS 195 (Antistax®).
Background: Chronic Venous Disorders or Diseases (CVD) of the lower extremities are a common finding affecting almost 90 % of an adult population. CVD includes varicose veins with a prevalence of approx. 25 %, overlapping with Chronic Venous Insufficiency (CVI) with a prevalence of approx. 17% in the adult population. CVI is characterized by venous pathology and objective signs like edema, skin changes or venous leg ulcers. Objective: To review and evaluate non-clinical and clinical data on a standardised herbal product containing flavonoids (AS195; Antistax®) and to put them into a perspective with the pathophysiology of CVD. Methods: Literature available on non-clinical pharmacology and clinical studies with AS195 in CVI of the lower extremities was reviewed and described. Conclusion: Antistax® is a well-described herbal product with standardised starting materials and manufacturing process. Its active ingredients accumulate in the venous intima, preserve the endothelial barrier function, and inhibit the inflammatory and prothrombotic cascade behind the progression of CVD. Its efficacy was analysed in adequately planned and executed clinical trials in patients with mild to moderately severe CVD (CEAP C1s to C4). AS195 showed a statistically significant and clinically relevant efficacy over placebo: in objective endpoints like volumetry of lower leg edema, but also in outcomes directly relevant for patients like tension and heaviness of the legs, tingling, and pain. Supportive studies confirmed and validated these results also for the broader population treated in daily practice. AS195 was well tolerated in studies and in everyday therapy. There are no known interactions with other medications. In the later stages, it can be used in combination with compression, complementing the beneficial haemodynamic effects of compression at a cellular level. AS195 is an addition to compression and closes a therapeutic gap especially in patients, who cannot use compression stockings, but still require CVD therapy.
Be well!
JP