Post Traumatic Stress Disorder Alternatives
March 7, 2011 Written by JP [Font too small?]Most people have endured one or more serious traumas in their lives. However, the extent of suffering and the exact definition placed on the word “trauma” vary greatly. What’s more, for reasons that aren’t entirely clear, certain individuals are more susceptible to the serious, long term consequences of trauma than others. Some survivors of abuse, assault, natural disasters and war develop a form of anxiety known as PTSD or post traumatic stress disorder. Symptoms of PTSD include emotional detachment, flashback episodes, memory loss, physical pain, recurrent nightmares, sleep disturbance and social withdrawal. Fortunately, some scientists are examining and finding success by utilizing select natural therapies in those living with traumatic memories.

A fascinating and groundbreaking study on PTSD was recently published in the journal Biopsychosocial Medicine. The paper describes a pilot study that evaluated the effects of fish oil supplementation in patients who were admitted to an intensive care unit after suffering physical trauma. The patients in question were administered a daily dosage of 1,470 mg of DHA and 147 mg of EPA, the two primary fatty acids contained in fish oil, for 12 weeks. The attending physicians noted that the fish oil was well tolerated and substantially reduced Clinician-Administered PTSD Scale (CAPS) scores compared to the expected scores of non-fish oil users in similar circumstances. Of the 15 patients tested, only one exhibited symptoms consistent with PTSD after undergoing the 12 week course of fish oil supplementation. The researchers went one step further and evaluated a potential mechanism to explain this promising finding. What they discovered is that the fish oil enhanced neurogenesis (brain cell development) in the hippocampal region of the brain by increasing a protein known as BDNF or brain-derived neurotrophic factor. The concluding remarks of the study noted that “omega-3 fatty acid supplementation immediately after accidental injury can reduce subsequent PTSD symptoms”. (1)
Combining exercise with conventional psychological interventions is also showing great promise in improving PTSD outcomes in various traumatized populations. The February 2011 issue of the journal Pain Medicine reports that the addition of “physical activity” to “biofeedback-based cognitive therapy” (CBT-BF) resulted in significantly better outcomes than using CBT-BF alone. The difference was quite profound: when exercise was included, a 60% success rate was reported. When cognitive therapy was used as an exclusive treatment option, the success rate was just 30%. What’s most important to note here is that this particular study examined both physical pain and psychological manifestations of trauma. In addition, these findings are backed up by several other trials involving animal models of PTSD and study populations ranging from male combat veterans to institutionalized, adolescent females. (2,3,4,5,6)
How Fish Oil May Protect Against PTSD
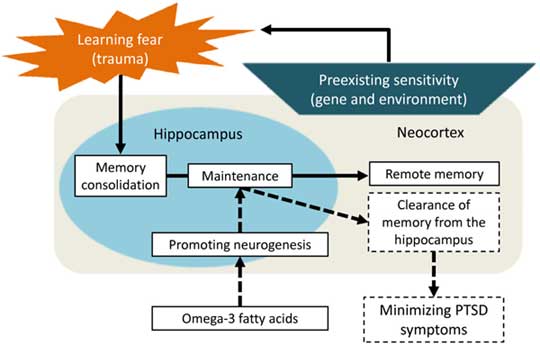
Source: BioPsychoSocial Medicine 2011, 5:3 (link)
Thought Field Therapy (TFT) is an unconventional mind-body technique that involves self-tapping with your fingers on specific acupressure points while thinking of emotionally disturbing or otherwise traumatic events. The concept behind TFT is that the simultaneous recalling and tapping process can unblock the flow of vital energy that may occur from negative experiences that are unresolved. Recent studies involving child genocide survivors suggest that this unorthodox approach may be an inexpensive and remarkably effective modality to consider for PTSD. In the Winter edition of the International Journal of Emergency Mental Health, “50 orphaned adolescents who had been suffering with symptoms of PTSD since the Rwandan genocide 12 years earlier” were treated with a single TFT session. At the start of the short-term experiment, 100% of the children were registered as having PTSD according to an assessment from their caregivers. After the TFT treatment that percentage dropped to 6%. Interviews with the caregivers and the study participants revealed a dramatic decline in aggression, bedwetting, depression, difficulty concentrating, flashbacks and isolating tendencies. Of note is that self-TFT treatment continued for a year following the study. The initial improvements were maintained and verified via caregiver and self-rated PTSD checklists. Other scientific inquiries on TFT involving traumatized “refugees and immigrants” and survivors of trauma in Kosovo also demonstrated a reduction in PTSD symptoms and protection against PTSD relapse. (7,8,9)
The first two options I presented today, fish oil supplementation and exercise, are unlikely to generate much controversy when used as adjuncts to conventional treatments such as cognitive behavioral therapy, pharmacological interventions and support groups. But, in both instances, a medical professional should be consulted in order to rule out potential side effects in some instances of physical trauma and/or prescriptive interactions. Thought Field Therapy is another matter altogether. There’s a fair share of skepticism in the mainstream psychological community about this unorthodox procedure. But, the fact of the matter is that it is possible to try TFT for free and test the results for yourself or, better yet, to do so with the assistance of a trained mental health professional. Nonprofit organizations such as the Association for Thought Field Therapy offer free assistance and information for anyone interested in learning more about Thought Field Therapy. All of this is to say that there is more hope now than ever before for those trying to overcome the damage caused by major traumas. (10)
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
Be well!
JP
Tags: Anxiety, Exercise, Fish Oil
Posted in Alternative Therapies, Mental Health, Nutritional Supplements

March 10th, 2011 at 10:08 pm
Wow, very interesting, JP!
March 10th, 2011 at 10:19 pm
Thanks a lot, Angie! 🙂
Be well!
JP
March 13th, 2011 at 12:29 pm
You should also check out the research Dr Upledger has done using Craniosacral Therapy for PTSD. I have had success using these techniques with clients who have suffered physical and emotional abuse who exhibited signs of PTSD.
I feel that although medications play a part in treatment, psychology and physiological therapies are an important part of restoring clients to full health.
March 13th, 2011 at 9:02 pm
Thank you, Michele. I appreciate the lead and your thoughtful insight. I’ll look into Craniosacral Therapy re: PTSD.
Be well!
JP
February 13th, 2014 at 10:50 pm
A new study showing the benefits of daily meditation practice: http://onlinelibrary.wiley.com/doi/10.1002/jts.21883/full
Be well!
JP
April 29th, 2015 at 2:29 pm
Update 04/29/15:
http://www.ncbi.nlm.nih.gov/pubmed/25915646
Psychol Trauma. 2015 Apr 27.
Mindfulness-Based Stress Reduction to Enhance Psychological Functioning and Improve Inflammatory Biomarkers in Trauma-Exposed Women: A Pilot Study.
This study examined the effects of a mindfulness-based stress reduction (MBSR) program on psychological functioning and inflammatory biomarkers in women with histories of interpersonal trauma. The 8-week MBSR program was conducted at a community-based health center and participants (N = 50) completed several measures of psychological functioning at study entry as well as 4 weeks, 8 weeks, and 12 weeks later. Inflammatory biomarkers were assayed from blood collected at each assessment. A series of linear mixed-model analyses were conducted to measure the effect of attendance and time on the dependent variables. Time was associated with significant decreases in perceived stress, depression, trait and state anxiety, emotion dysregulation, and posttraumatic stress symptoms, as well as increases in mindfulness. Session attendance was associated with significant decreases in interleukin (IL)-6 levels. This pilot study demonstrated the potential beneficial effects of MBSR on psychological functioning and the inflammatory biomarker IL-6 among trauma-exposed and primarily low-income women. Decreases in inflammation have implications for this population, as interpersonal trauma can instigate chronic physiological dysregulation, heightened morbidity, and premature death. This study’s preliminary results support efforts to investigate biological remediation with behavioral interventions in vulnerable populations.
Be well!
JP
May 25th, 2015 at 6:33 pm
Update 05/25/15:
http://www.ncbi.nlm.nih.gov/pubmed/25989952
Eur J Psychotraumatol. 2015 May 18;6:27414.
EMDR for Syrian refugees with posttraumatic stress disorder symptoms: results of a pilot randomized controlled trial.
BACKGROUND: The most common mental health problems among refugees are depression and posttraumatic stress disorder (PTSD). Eye movement desensitization and reprocessing (EMDR) is an effective treatment for PTSD. However, no previous randomized controlled trial (RCT) has been published on treating PTSD symptoms in a refugee camp population.
OBJECTIVE: Examining the effect of EMDR to reduce the PTSD and depression symptoms compared to a wait-list condition among Syrian refugees.
METHOD: Twenty-nine adult participants with PTSD symptoms were randomly allocated to either EMDR sessions (n=15) or wait-list control (n=14). The main outcome measures were Impact of Event Scale-Revised (IES-R) and Beck Depression Inventory (BDI-II) at posttreatment and 4-week follow-up.
RESULTS: Analysis of covariance showed that the EMDR group had significantly lower trauma scores at posttreatment as compared with the wait-list group (d=1.78, 95% CI: 0.92-2.64). The EMDR group also had a lower depression score after treatment as compared with the wait-list group (d=1.14, 95% CI: 0.35-1.92).
CONCLUSION: The pilot RCT indicated that EMDR may be effective in reducing PTSD and depression symptoms.
Be well!
JP
May 25th, 2015 at 6:37 pm
Update 05/25/15:
http://online.liebertpub.com/doi/10.1089/acm.2014.0389
J Altern Complement Med. 2015 May 14.
Impact of a Yoga Intervention on Physical Activity, Self-Efficacy, and Motivation in Women with PTSD Symptoms.
BACKGROUND: Studies using yoga have demonstrated initial efficacy for treating symptoms across anxiety disorders, including post-traumatic stress disorder.
OBJECTIVE: Understanding how interventions influence participants’ physical activity and what determinants affect continued physical activity behavior change is important because maintenance of the behavior may be critical to continued mental health gains and symptom reduction.
METHODS: This study investigated change in physical activity and possible psychological mechanisms of physical activity behavior change, including self-efficacy and regulatory motivation, in a randomized controlled trial of yoga for women with post-traumatic stress disorder symptoms (n=38).
RESULTS: Growth curve modeling results showed no significant changes in physical activity or self-efficacy for either group, whereas external motivation decreased significantly in the yoga group but not in the control group.
CONCLUSIONS: Investigators of future yoga interventions may want to focus on increasing self-efficacy and internal regulatory motivation, so that physical activity and resultant symptom relief can be maintained.
Be well!
JP
July 8th, 2015 at 1:30 pm
Update 07/08/15:
http://www.ncbi.nlm.nih.gov/pubmed/26149677
J Interpers Violence. 2015 Jul 5.
Impact of Meditation on Mental Health Outcomes of Female Trauma Survivors of Interpersonal Violence With Co-Occurring Disorders: A Randomized Controlled Trial.
This study was a randomized controlled trial that examined the impact of meditation practice on the mental health outcomes of female trauma survivors of interpersonal violence who have co-occurring disorders. Sixty-three female trauma survivors were randomly assigned to the meditation condition and the control condition. Treatment conditions consisted of a 6-week meditation curriculum that was influenced by Tibetan meditation tradition and focused on breathing, loving kindness, and compassion meditation. Clients in the meditation condition made significant changes in mental health symptoms (t = 5.252, df = 31, p = .000) and trauma symptoms (t = 6.009, df = 31, p = .000) from pre-treatment to post-treatment, whereas non-significant changes were observed among the control condition clients. There were significant group differences between clients in the meditation condition and in the control condition on their mental health symptoms, F(1, 54) = 13.438, p = .001, and trauma symptoms, F(1, 54) = 13.395, p = .001, with a generally large effect size of eta squared .127 and .146, respectively. In addition, significantly more clients in the meditation condition achieved reliable change in mental health symptoms (35.5% vs. 8.3%) and trauma symptoms (42.3% vs. 4.8%) than clients in the control condition. Significance of the study is discussed with respect to the empirical evidence of meditation practice as a complementary behavioral intervention for treating female trauma survivors of interpersonal violence who have co-occurring disorders.
Be well!
JP
July 14th, 2015 at 3:18 pm
Update 07/14/15:
http://www.ncbi.nlm.nih.gov/pubmed/26153191
Glob J Health Sci. 2015 Apr 19;7(6):47723.
Effect of Eye Movement Desensitization and Reprocessing (EMDR) on Depression in Patients With Myocardial Infarction (MI).
BACKGROUND: Coronary heart disease is the most important cause of death and inability in all communities. Depressive symptoms are frequent among post-myocardial infarction (MI) patients and may cause negative effects on cardiac prognosis. This study was conducted to identify efficacy of EMDR on depression of patients with MI.
METHODS: This study is a clinical trial. Sixty patients with MI were selected by simple sampling, and were separated randomly into experimental and control groups. To collect data, demographic questionnaire and Beck Depression Questionnaire were used. In experimental group, EMDR therapy were performed in three sessions alternate days for 45-90 minutes, during four months after their MI. Depression level of patients was measured before, and a week after EMDR therapy. Data were analyzed using paired -t- test, t-test, and Chi-square.
RESULTS: The mean depression level in experimental group 27.26± 6.41 before intervention, and it was 11.76 ± 3.71 after intervention. Hence, it showed a statistically significant difference (P<0.001). The mean depression level in control group was 24.53 ± 5.81 before intervention, and it was 31.66± 6.09 after intervention, so it showed statistically significant difference (P<0.001). The comparison of mean depression level at post treatment, in both groups showed statistically significant difference (P<0.001).
CONCLUSION: EMDR is an effective, useful, efficient, and non-invasive method for treatment and reducing depression in patients with MI.
Be well!
JP
August 5th, 2015 at 2:31 pm
Updated 08/05/15:
http://www.ncbi.nlm.nih.gov/pubmed/26241597
JAMA. 2015 Aug 4;314(5):456-465.
Mindfulness-Based Stress Reduction for Posttraumatic Stress Disorder Among Veterans: A Randomized Clinical Trial.
Importance: Mindfulness-based interventions may be acceptable to veterans who have poor adherence to existing evidence-based treatments for posttraumatic stress disorder (PTSD).
Objective: To compare mindfulness-based stress reduction with present-centered group therapy for treatment of PTSD.
Design, Setting, and Participants: Randomized clinical trial of 116 veterans with PTSD recruited at the Minneapolis Veterans Affairs Medical Center from March 2012 to December 2013. Outcomes were assessed before, during, and after treatment and at 2-month follow-up. Data collection was completed on April 22, 2014.
Interventions: Participants were randomly assigned to receive mindfulness-based stress reduction therapy (n = 58), consisting of 9 sessions (8 weekly 2.5-hour group sessions and a daylong retreat) focused on teaching patients to attend to the present moment in a nonjudgmental, accepting manner; or present-centered group therapy (n = 58), an active-control condition consisting of 9 weekly 1.5-hour group sessions focused on current life problems.
Main Outcomes and Measures: The primary outcome, change in PTSD symptom severity over time, was assessed using the PTSD Checklist (range, 17-85; higher scores indicate greater severity; reduction of 10 or more considered a minimal clinically important difference) at baseline and weeks 3, 6, 9, and 17. Secondary outcomes included PTSD diagnosis and symptom severity assessed by independent evaluators using the Clinician-Administered PTSD Scale along with improvements in depressive symptoms, quality of life, and mindfulness.
Results: Participants in the mindfulness-based stress reduction group demonstrated greater improvement in self-reported PTSD symptom severity during treatment (change in mean PTSD Checklist scores from 63.6 to 55.7 vs 58.8 to 55.8 with present-centered group therapy; between-group difference, 4.95; 95% CI, 1.92-7.99; P=.002) and at 2-month follow-up (change in mean scores from 63.6 to 54.4 vs 58.8 to 56.0, respectively; difference, 6.44; 95% CI, 3.34-9.53, P < .001). Although participants in the mindfulness-based stress reduction group were more likely to show clinically significant improvement in self-reported PTSD symptom severity (48.9% vs 28.1% with present-centered group therapy; difference, 20.9%; 95% CI, 2.2%-39.5%; P = .03) at 2-month follow-up, they were no more likely to have loss of PTSD diagnosis (53.3% vs 47.3%, respectively; difference, 6.0%; 95% CI, -14.1% to 26.2%; P = .55). Conclusions and Relevance: Among veterans with PTSD, mindfulness-based stress reduction therapy, compared with present-centered group therapy, resulted in a greater decrease in PTSD symptom severity. However, the magnitude of the average improvement suggests a modest effect. Be well! JP
November 11th, 2015 at 1:02 pm
Updated 11/11/15:
http://jhn.sagepub.com/content/early/2015/11/02/0898010115610050.abstract
J Holist Nurs. 2015 Nov 3.
Exploring Self-Reported Benefits of Auricular Acupuncture Among Veterans With Posttraumatic Stress Disorder.
PURPOSE: Auricular acupuncture treatments are becoming increasingly available within military treatment facilities, resulting in an expansion of nonpharmacologic treatment options available to veterans with posttraumatic stress disorder (PTSD). This study aimed to explore the self-reported benefits of auricular acupuncture treatments for veterans living with PTSD.
DESIGN: A qualitative research methodology, thematic content analysis, was used to analyze data.
METHOD: Seventeen active duty veterans with PTSD provided written comments to describe their experiences and perceptions after receiving a standardized auricular acupuncture regimen for a 3-week period as part of a pilot feasibility study.
FINDINGS: A variety of symptoms experienced by veterans with PTSD were improved after receiving auricular acupuncture treatments. Additionally, veterans with PTSD were extremely receptive to auricular acupuncture treatments. Four themes emerged from the data: (1) improved sleep quality, (2) increased relaxation, (3) decreased pain, and (4) veterans liked/loved the auricular acupuncture treatments.
CONCLUSIONS: Veterans with PTSD reported numerous benefits following auricular acupuncture treatments. These treatments may facilitate healing and recovery for veterans with combat-related PTSD, although further investigations are warranted into the mechanisms of action for auricular acupuncture in this population.
Be well!
JP
January 8th, 2016 at 11:23 pm
Updated 1/8/16:
http://www.ncbi.nlm.nih.gov/pubmed/26741477
Mil Med. 2016 Jan;181(1):56-63.
Impact of Transcendental Meditation on Psychotropic Medication Use Among Active Duty Military Service Members With Anxiety and PTSD.
The purpose of the study was to determine whether the regular practice of Transcendental Meditation (TM) decreased the need for psychotropic medications required for anxiety and post-traumatic stress disorder (PTSD) management and increased psychological wellbeing. The sample included 74 military Service Members with documented PTSD or anxiety disorder not otherwise specified (ADNOS), 37 that practiced TM and 37 that did not. At 1 month, 83.7% of the TM group stabilized, decreased, or ceased medications and 10.8% increased medication dosage; compared with 59.4% of controls that showed stabilizations, decreases, or cessations; and 40.5% that increased medications (p < 0.03). A similar pattern was observed after 2 (p < 0.27), 3 (p < 0.002), and 6 months (p < 0.34). Notably, there was a 20.5% difference between groups in severity of psychological symptoms after 6 months, that is, the control group experienced an increase in symptom severity compared with the group practicing TM. These findings provide insight into the benefits of TM as a viable treatment modality in military treatment facilities for reducing PTSD and ADNOS psychological symptoms and associated medication use. Be well! JP
March 19th, 2016 at 5:43 pm
Updated 03/19/16:
http://www.ncbi.nlm.nih.gov/pubmed/26934487
J Trauma Stress. 2016 Mar 2.
The Effectiveness of Eye Movement Desensitization and Reprocessing Therapy to Treat Symptoms Following Trauma in Timor Leste.
The effectiveness of eye movement desensitization and reprocessing (EMDR) therapy for treating trauma symptoms was examined in a postwar/conflict, developing nation, Timor Leste. Participants were 21 Timorese adults with symptoms of posttraumatic stress disorder (PTSD), assessed as those who scored ≥2 on the Harvard Trauma Questionnaire (HTQ). Participants were treated with EMDR therapy. Depression and anxiety symptoms were assessed using the Hopkins Symptom Checklist. Symptom changes post-EMDR treatment were compared to a stabilization control intervention period in which participants served as their own waitlist control. Sessions were 60-90 mins. The average number of sessions was 4.15 (SD = 2.06). Despite difficulties providing treatment cross-culturally (i.e., language barriers), EMDR therapy was followed by significant and large reductions in trauma symptoms (Cohen’s d = 2.48), depression (d = 2.09), and anxiety (d = 1.77). At posttreatment, 20 (95.2%) participants scored below the HTQ PTSD cutoff of 2. Reliable reductions in trauma symptoms were reported by 18 participants (85.7%) posttreatment and 16 (76.2%) at 3-month follow-up. Symptoms did not improve during the control period. Findings support the use of EMDR therapy for treatment of adults with PTSD in a cross-cultural, postwar/conflict setting, and suggest that structured trauma treatments can be applied in Timor Leste.
Be well!
JP
May 6th, 2016 at 12:45 pm
Updated 05/06/16:
http://www.ncbi.nlm.nih.gov/pubmed/27148134
Front Psychol. 2016 Apr 21;7:526.
Treating Post-traumatic Stress Disorder in Patients with Multiple Sclerosis: A Randomized Controlled Trial Comparing the Efficacy of Eye Movement Desensitization and Reprocessing and Relaxation Therapy.
OBJECTIVE: Multiple Sclerosis (MS) is a demyelinating autoimmune disease that imposes a significant emotional burden with heavy psychosocial consequences. Several studies have investigated the association between MS and mental disorders such as depression and anxiety, and recently researchers have focused also on Post-traumatic Stress Disorder (PTSD). This is the first study that investigates the usefulness of proposing a treatment for PTSD to patients with MS.
METHODS: A randomized controlled trial with patients with MS diagnosed with PTSD comparing Eye Movement Desensitization and Reprocessing (EMDR; n = 20) and Relaxation Therapy (RT; n = 22). The primary outcome measure was the proportion of participants that no longer meet PTSD diagnosis as measured with Clinician Administered PTSD Scale 6-months after the treatment.
RESULTS: The majority of patients were able to overcome their PTSD diagnosis after only 10 therapy sessions. EMDR treatment appears to be more effective than RT in reducing the proportion of patients with MS suffering from PTSD. Both treatments are effective in reducing PTSD severity, anxiety and depression symptoms, and to improve Quality of Life.
CONCLUSION: Although our results can only be considered preliminary, this study suggests that it is essential that PTSD symptoms are detected and that brief and cost-effective interventions to reduce PTSD and associated psychological symptoms are offered to patients, in order to help them to reduce the psychological burden associated with their neurological condition.
Be well!
JP
June 12th, 2016 at 10:33 pm
Updated 06/12/16:
http://www.ncbi.nlm.nih.gov/pubmed/27287561
J Affect Disord. 2016 May 30.
Effects of omega-3 polyunsaturated fatty acids on psychophysiological symptoms of post-traumatic stress disorder in accident survivors: A randomized, double-blind, placebo-controlled trial.
BACKGROUND: Psychophysiological symptoms (e.g., pounding heart) are known to be a prominent feature of post-traumatic stress disorder (PTSD). Although omega-3 polyunsaturated fatty acids (PUFAs) have a beneficial potential pharmacological effect of preventing these psychophysiological symptoms, no clinical data is yet available. Therefore, we conducted a randomized, double-blind, placebo-controlled trial of Japanese accident survivors.
METHODS: A total of 83 participants received either omega-3 PUFAs (1470mg docosahexaenoic acid and 147mg eicosapentaenoic acid per day) or placebo within 10 days of the accidental injury. After 12-week supplementation, participants performed script-driven imagery of their traumatic event during monitoring of their heart rate and skin conductance.
RESULTS: Analysis revealed that heart rate during both rest and script-driven imagery was significantly lower in the omega-3 group than the placebo group, whereas baseline heart rate was comparable between the two groups.
LIMITATIONS: The present trial was conducted at a single-center in Japan and psychophysiological symptoms of PTSD in most participants were not serious.
CONCLUSION: These findings suggest that post-trauma supplementation of omega-3 PUFAs might be effective for the secondary prevention of psychophysiological symptoms of PTSD.
Be well!
JP
August 22nd, 2016 at 2:42 pm
Updated 08/22/16:
http://www.ncbi.nlm.nih.gov/pubmed/27543343
Explore (NY). 2016 Jun 27.
EFT (Emotional Freedom Techniques) and Resiliency in Veterans at Risk for PTSD: A Randomized Controlled Trial.
Prior research indicates elevated but subclinical posttraumatic stress disorder (PTSD) symptoms as a risk factor for a later diagnosis of PTSD. This study examined the progression of symptoms in 21 subclinical veterans. Participants were randomized into a treatment as usual (TAU) wait-list group and an experimental group, which received TAU plus six sessions of clinical emotional freedom techniques (EFT). Symptoms were assessed using the PCL-M (Posttraumatic Checklist-Military) on which a score of 35 or higher indicates increased risk for PTSD. The mean pretreatment score of participants was 39 ± 8.7, with no significant difference between groups. No change was found in the TAU group during the wait period. Afterward, the TAU group received an identical clinical EFT protocol. Posttreatment groups were combined for analysis. Scores declined to a mean of 25 (-64%, P < .0001). Participants maintained their gains, with mean three-month and six-month follow-up PCL-M scores of 27 (P < .0001). Similar reductions were noted in the depth and breadth of psychological conditions such as anxiety. A Cohen's d = 1.99 indicates a large treatment effect. Reductions in traumatic brain injury symptoms (P = .045) and insomnia (P = .004) were also noted. Symptom improvements were similar to those assessed in studies of PTSD-positive veterans. EFT may thus be protective against an increase in symptoms and a later PTSD diagnosis. As a simple and quickly learned self-help method, EFT may be a clinically useful element of a resiliency program for veterans and active-duty warriors. Be well! JP
August 28th, 2016 at 5:36 pm
Updated 08/28/16:
http://www.jad-journal.com/article/S0165-0327(16)30041-6/abstract
J Affect Disord. 2016 Aug 16;205:351-359.
Fatty acid concentrations in patients with posttraumatic stress disorder compared to healthy controls.
BACKGROUND: Although fatty acid (FA)-supplementation studies are currently being implemented, in fact little is known about FA-profiles in posttraumatic stress disorder (PTSD). Therefore, the present study aimed at comparing FA-concentrations between PTSD-patients and healthy controls.
METHODS: A cross-sectional study comparing a mixed-gender sample of 49 patients with PTSD due to civilian trauma to 46 healthy controls regarding erythrocyte FAs including docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), arachidonic acid (AA), and nervonic acid (NA).
RESULTS: DHA was found to be significantly lower in PTSD-patients compared to controls after adjusting for sociodemographic and dietary factors (p =0.043). Additionally, exploratory analyses showed lower vaccenic acid (p =0.035) and eicosatrienoic acid (p =0.006), but higher erucic acid (p =0.032) in PTSD-patients. The effect of erucic acid remained after adjustment for sociodemographic factors (p =0.047); with the additional adjustment for dietary factors none of these FAs were found to be significant.
LIMITATIONS: Statistical power for differences with small effect sizes was limited, and dietary assessment could be optimized.
CONCLUSIONS: We found little evidence for a considerable role of FA-metabolism in PTSD. Apart from lower DHA after adjusting for confounders, no differences were observed in the hypothesized long-chained polyunsaturated FA-concentrations. Additionally, we found few alterations in the long-chained monounsaturated FAs, which may be explained by dietary factors. Nevertheless, the observed small effect sizes and limited extent of the alterations emphasize the importance of further investigating the assumed role of FA-metabolism and its underlying mechanisms in PTSD, before implementing further FA-supplementation studies.
Be well!
JP
September 25th, 2016 at 1:40 pm
Updated 09/25/16:
https://www.sciencedaily.com/releases/2016/09/160922104406.htm
Fish Oil May Help Improve Mood in Veterans
Source: Texas A&M University
Summary: Low concentration of fish oil in the blood and lack of physical activity may contribute to the high levels of depressed mood among soldiers returning from combat, according to researchers.
Be well!
JP
November 2nd, 2016 at 1:12 pm
Updated 11/02/16:
http://www.psychiatrist.com/JCP/article/Pages/2016/aheadofprint/15m10239.aspx
J Clin Psychiatry. 2016 Oct 11.
A Double-Blind, Randomized, Controlled Pilot Trial of N-Acetylcysteine in Veterans With Posttraumatic Stress Disorder and Substance Use Disorders.
OBJECTIVE: The antioxidant N-acetylcysteine is being increasingly investigated as a therapeutic agent in the treatment of substance use disorders (SUDs). This study explored the efficacy of N-acetylcysteine in the treatment of posttraumatic stress disorder (PTSD), which frequently co-occurs with SUD and shares impaired prefrontal cortex regulation of basal ganglia circuitry, in particular at glutamate synapses in the nucleus accumbens.
METHODS: Veterans with PTSD and SUD per DSM-IV criteria (N = 35) were randomly assigned to receive a double-blind, 8-week course of N-acetylcysteine (2,400 mg/d) or placebo plus cognitive-behavioral therapy for SUD (between March 2013 and April 2014). Primary outcome measures included PTSD symptoms (Clinician-Administered PTSD Scale, PTSD Checklist-Military) and craving (Visual Analog Scale). Substance use and depression were also assessed.
RESULTS: Participants treated with N-acetylcysteine compared to placebo evidenced significant improvements in PTSD symptoms, craving, and depression (β values < -0.33; P values < .05). Substance use was low for both groups, and no significant between-group differences were observed. N-acetylcysteine was well tolerated, and retention was high. CONCLUSIONS: This is the first randomized controlled trial to investigate N-acetylcysteine as a pharmacologic treatment for PTSD and SUD. Although preliminary, the findings provide initial support for the use of N-acetylcysteine in combination with psychotherapy among individuals with co-occurring PTSD and SUD. Be well! JP
June 9th, 2017 at 11:41 am
Updated 06/09/17:
http://www.jad-journal.com/article/S0165-0327(16)30239-7/abstract
J Affect Disord. 2016 May 30.
Effects of omega-3 polyunsaturated fatty acids on psychophysiological symptoms of post-traumatic stress disorder in accident survivors: A randomized, double-blind, placebo-controlled trial.
BACKGROUND: Psychophysiological symptoms (e.g., pounding heart) are known to be a prominent feature of post-traumatic stress disorder (PTSD). Although omega-3 polyunsaturated fatty acids (PUFAs) have a beneficial potential pharmacological effect of preventing these psychophysiological symptoms, no clinical data is yet available. Therefore, we conducted a randomized, double-blind, placebo-controlled trial of Japanese accident survivors.
METHODS: A total of 83 participants received either omega-3 PUFAs (1470mg docosahexaenoic acid and 147mg eicosapentaenoic acid per day) or placebo within 10 days of the accidental injury. After 12-week supplementation, participants performed script-driven imagery of their traumatic event during monitoring of their heart rate and skin conductance.
RESULTS: Analysis revealed that heart rate during both rest and script-driven imagery was significantly lower in the omega-3 group than the placebo group, whereas baseline heart rate was comparable between the two groups.
LIMITATIONS: The present trial was conducted at a single-center in Japan and psychophysiological symptoms of PTSD in most participants were not serious.
CONCLUSION: These findings suggest that post-trauma supplementation of omega-3 PUFAs might be effective for the secondary prevention of psychophysiological symptoms of PTSD.
Be well!
JP
September 12th, 2017 at 12:53 pm
Updated 09/12/17:
https://www.ncbi.nlm.nih.gov/pubmed/28890702
Front Psychiatry. 2017 Aug 25;8:157.
A Pilot Study of the Effects of Mindfulness-Based Stress Reduction on Post-traumatic Stress Disorder Symptoms and Brain Response to Traumatic Reminders of Combat in Operation Enduring Freedom/Operation Iraqi Freedom Combat Veterans with Post-traumatic Stress Disorder.
OBJECTIVE: Brain imaging studies in patients with post-traumatic stress disorder (PTSD) have implicated a circuitry of brain regions including the medial prefrontal cortex, amygdala, hippocampus, parietal cortex, and insula. Pharmacological treatment studies have shown a reversal of medial prefrontal deficits in response to traumatic reminders. Mindfulness-based stress reduction (MBSR) is a promising non-pharmacologic approach to the treatment of anxiety and pain disorders. The purpose of this study was to assess the effects of MBSR on PTSD symptoms and brain response to traumatic reminders measured with positron-emission tomography (PET) in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) combat veterans with PTSD. We hypothesized that MBSR would show increased prefrontal response to stress and improved PTSD symptoms in veterans with PTSD.
METHOD: Twenty-six OEF/OIF combat veterans with PTSD who had recently returned from a combat zone were block randomized to receive eight sessions of MBSR or present-centered group therapy (PCGT). PTSD patients underwent assessment of PTSD symptoms with the Clinician-Administered PTSD Scale (CAPS), mindfulness with the Five Factor Mindfulness Questionnaire (FFMQ) and brain imaging using PET in conjunction with exposure to neutral and Iraq combat-related slides and sound before and after treatment. Nine patients in the MBSR group and 8 in the PCGT group completed all study procedures.
RESULTS: Post-traumatic stress disorder patients treated with MBSR (but not PCGT) had an improvement in PTSD symptoms measured with the CAPS that persisted for 6 months after treatment. MBSR also resulted in an increase in mindfulness measured with the FFMQ. MBSR-treated patients had increased anterior cingulate and inferior parietal lobule and decreased insula and precuneus function in response to traumatic reminders compared to the PCGT group.
CONCLUSION: This study shows that MBSR is a safe and effective treatment for PTSD. Furthermore, MBSR treatment is associated with changes in brain regions that have been implicated in PTSD and are involved in extinction of fear responses to traumatic memories as well as regulation of the stress response.
Be well!
JP
November 28th, 2017 at 2:40 pm
Updated 11/28/17:
http://journals.sagepub.com/doi/pdf/10.1177/0898010117697617
J Holist Nurs. 2017 Mar 1:898010117697617.
Tai Chi for Posttraumatic Stress Disorder and Chronic Musculoskeletal Pain: A Pilot Study.
PURPOSE: Explore the feasibility of a Tai Chi intervention to improve musculoskeletal pain, emotion, cognition, and physical function in individuals with posttraumatic stress disorder.
DESIGN: Two-phase, one-arm quasi-experimental design.
METHOD: Phase 1: 11 participants completed one Tai Chi session, feasibility questionnaire, and were offered participation in Phase 2, a 12-week Tai Chi intervention. Ten participants participated in Phase 2. Pain intensity, interference, physical function scales, an emotional battery, and cognition tests were used for pre- and postintervention outcome measures. Paired t tests and thematic analysis were used for analysis.
FINDINGS: In Phase 1, most felt Tai Chi would benefit health (90.9%) and expressed interest in continuing Tai Chi (6.73 out of 7). Phase 2 results showed improvement in fear-affect (raw t = -2.64, p = .03; age adjusted t = -2.90, p = .02), fear-somatic arousal (raw t = -2.53, p = .035), List Sorting Working Memory (raw t = 2.62, p = .031; age adjusted t = 2.96, p = .018), 6-Minute Walk Test ( t = 3.541, p = .008), and current level of Pain Intensity ( t = -4.00, p = .004).
CONCLUSIONS: Tai Chi is an acceptable, holistic treatment to individuals with musculoskeletal pain and posttraumatic stress disorder. It may reduce pain, improve emotion, memory, and physical function.
Be well!
JP
February 6th, 2018 at 1:49 pm
Updated 2/6/18:
https://www.ncbi.nlm.nih.gov/pubmed/29401353
Mil Med. 2018 Jan 1;183(1-2):e144-e150.
The Transcendental Meditation Program’s Impact on the Symptoms of Post-traumatic Stress Disorder of Veterans: An Uncontrolled Pilot Study.
Background: Current treatments for post-traumatic stress disorder (PTSD) are only partially effective. This study evaluated whether an extensively researched stress reduction method, the Transcendental Meditation (TM) technique, can reduce the PTSD symptoms of veterans. Previous research suggested that TM practice can decrease veterans’ PTSD symptoms.
Methods: A one-group pretest-posttest design was used to evaluate the impact of TM practice on reducing PTSD symptoms. A convenience sample of 89 veterans completed PTSD Checklist-Civilian (PCL-5) questionnaires. Among those, 46 scored above 33, the threshold for provisional diagnosis of PTSD, and were included in this evaluation. The PCL-5 measured PTSD symptoms at baseline and 30 and 90 d after intervention. Regularity of TM practice was recorded. Paired sample t-tests were used to assess within-group changes from baseline to post-intervention periods. Analysis of variance was used to compare full-dose (two 20-min TM sessions per day) and half-dose (one 20-min TM session per day) groups.
Findings: After 1 mo of TM practice, all 46 veterans responded; their PCL-5 average decreased from 51.52 in the pre-intervention period to a post-intervention mean of 23.43, a decline of 28.09 points (-54.5%); standard deviation: 14.57; confidence interval: 23.76-32.41; and effect size: -1.93; p < 0.0001. The median PTSD scores declined from 52.5 to 22.5, a decrease of 30 points (-57%), while 40 veterans (87%) had clinically significant declines (>10 points) in PTSD symptoms, and 37 (80%) dropped below the clinical level (<33). At the 90 d posttest, 31 of the 46 responded and three more dropped below the 33 threshold. Intent-to-treat analyses revealed clinically and statistically significant effects. A dose-response effect suggested a causal relationship. The full-dose group exhibited larger mean declines in PTSD symptoms than the half-dose group. Averages of the 46 veterans' responses to 20 PCL-5 questions exhibited significant (p < 0.0001) declines from the pre-intervention period to the 30-d post-intervention assessment. Discussion: Results indicated that TM practice reduced PTSD symptoms without re-experiencing trauma. Because of the magnitude of these results and dose-response effect, regression to the mean, spontaneous remission of symptoms, and placebo effects are unlikely explanations for the results. Major limitations were absence of random assignment and lack of a control group. Participants chose to start and continue TM practice and to complete PCL-5 questionnaires. Those who self-selected to enter this study may not be representative of all veterans who have PTSD. Those who did not complete follow-up questionnaires at 90 d may or may not have had the same results as those who responded. The design and sampling method affect the generalizability of the results to wider populations. When taking into account these results and all previous research on the TM technique in reducing psychological and physiological stress, the convergence of evidence suggests that TM practice may offer a promising adjunct or alternative method for treating PTSD. Because of the widely recognized need to identify effective new approaches for treating PTSD, randomized research with control groups is warranted to further investigate the effectiveness of TM practice as a treatment for PTSD. Be well! JP
September 27th, 2018 at 11:56 am
Updated 09/27/18:
https://www.ncbi.nlm.nih.gov/pubmed/30256652
J Altern Complement Med. 2018 Sep 25.
Dog Ownership and Training Reduces Post-Traumatic Stress Symptoms and Increases Self-Compassion Among Veterans: Results of a Longitudinal Control Study.
OBJECTIVES: The aims of this study were to measure the potential impact of a therapeutic dog ownership and training program for Veterans with symptoms of post-traumatic stress.
DESIGN: The study used a quasi-experimental design with two cohorts of Veterans-a dog owner-trainer intervention and a wait list control group. Participants completed baseline and 12-month follow-up assessments.
SETTING: Clear Path for Veterans, a nonclinical, open recreation facility whose mission is to support Veterans and their families in the reintegration process after military service.
SUBJECTS: Participants (n = 48) were either enrolled in the veterans therapeutic dog owner-trainer program (Dogs2Vets) or were placed in the wait list control group.
INTERVENTION: Veterans were enrolled in the Dogs2Vets program, a 12-month structured dog owner-trainer program that engages veterans in the training and care of a dog that they ultimately adopt. The Dogs2Vets Program focuses on the healing aspects of the human-animal bond.
OUTCOME MEASURES: PTSD Checklist, Military Version (PCL-M), perceived stress scale, self-compassion scale (SCS) composite, and SCS subscales for isolation and self-judgment.
RESULTS: Veterans participating in the Dogs2Vets owner-trainer program experienced significant reductions in symptoms of post-traumatic stress, perceived stress, isolation, and self-judgment accompanied by significant increases in self-compassion. In contrast there were no significant improvements in these measures among veterans in the wait list control group. Qualitative data reinforced the statistical findings with themes of decreased isolation, unconditional acceptance and companionship, and a renewed sense of safety and purpose from their relationships with their dogs.
CONCLUSION: Veterans benefit significantly from dog ownership in combination with a structured dog training program. Not only do they experience significant decreases in stress and post-traumatic stress symptoms but also they experience less isolation and self-judgment while also experiencing significant improvements in self-compassion.
Be well!
JP
November 27th, 2018 at 1:10 pm
Updated 11/27/18:
https://jkms.org/DOIx.php?id=10.3346/jkms.2018.33.e306
J Korean Med Sci. 2018 Nov 5;33(48):e306.
Add-on Eye Movement Desensitization and Reprocessing (EMDR) Therapy for Adults with Post-traumatic Stress Disorder Who Failed to Respond to Initial Antidepressant Pharmacotherapy.
This study examined the add-on efficacy of eye movement desensitization and reprocessing (EMDR) therapy among adult civilians with post-traumatic stress disorder (PTSD) who continued to be symptomatic after more than 12 weeks of initial antidepressant treatment. Scores for the Clinician Administered PTSD Scale (CAPS) were rated pre- and post-EMDR and at a 6-month follow-up. After an average of six sessions of EMDR treatment, seven of 14 patients (50%) showed more than a 30% decrease in CAPS score and eight (57%) no longer met the criteria for PTSD. Our results indicate that EMDR could be successfully added after failure of initial pharmacotherapy for PTSD.
Be well!
JP
December 14th, 2018 at 1:30 pm
Updated 12/14/18:
https://www.liebertpub.com/doi/10.1089/acm.2018.0437
J Altern Complement Med. 2018 Dec 13.
Cannabidiol in the Treatment of Post-Traumatic Stress Disorder: A Case Series.
OBJECTIVES: Cannabidiol (CBD) is a non-psychotomimetic cannabinoid compound that is found in plants of the genus Cannabis. Preclinical research has suggested that CBD may have a beneficial effect in rodent models of post-traumatic stress disorder (PTSD). This effect is believed to be due to the action of CBD on the endocannabinoid system. CBD has seen a recent surge in research regarding its potential value in a number of neuro-psychiatric conditions. This is the first study to date examining the clinical benefit of CBD for patients with PTSD.
METHODS: This retrospective case series examines the effect of oral CBD administration on symptoms of PTSD in a series of 11 adult patients at an outpatient psychiatry clinic. CBD was given on an open-label, flexible dosing regimen to patients diagnosed with PTSD by a mental health professional. Patients also received routine psychiatric care, including concurrent treatment with psychiatric medications and psychotherapy. The length of the study was 8 weeks. PTSD symptom severity was assessed every 4 weeks by patient-completed PTSD Checklist for the DSM-5 (PCL-5) questionnaires.
RESULTS: From the total sample of 11 patients, 91% (n = 10) experienced a decrease in PTSD symptom severity, as evidenced by a lower PCL-5 score at 8 weeks than at their initial baseline. The mean total PCL-5 score decreased 28%, from a mean baseline score of 51.82 down to 37.14, after eight consecutive weeks of treatment with CBD. CBD was generally well tolerated, and no patients discontinued treatment due to side effects.
CONCLUSIONS: Administration of oral CBD in addition to routine psychiatric care was associated with PTSD symptom reduction in adults with PTSD. CBD also appeared to offer relief in a subset of patients who reported frequent nightmares as a symptom of their PTSD. Additional clinical investigation, including double-blind, placebo-controlled trials, would be necessary to further substantiate the response to CBD that was observed in this study.
Be well!
JP
February 19th, 2019 at 3:54 pm
Updated 02/19/19:
https://www.tandfonline.com/doi/abs/10.1080/19390211.2019.1572040?journalCode=ijds20
J Diet Suppl. 2019 Feb 18:1-9.
Comparing Perika St. John’s Wort and Sertraline for Treatment of Posttraumatic Stress Disorder in Mice.
Posttraumatic stress disorder (PTSD) is a serious mental health condition that affects some individuals who have witnessed or experienced a life-threatening or traumatic event. An enhanced or exaggerated acoustic startle response (ASR), reflecting heightened sensitivity to unexpected, loud sound, is a hallmark symptom of PTSD. Antidepressant medications, such as sertraline, are first-line pharmacotherapeutic agents in the treatment of PTSD, but concerns about potential side effects or taking synthetic drugs prompt discovery of naturalistic therapeutic agents. This study examined the relative effectiveness of a compound containing St. John’s Wort (SJW), an herb widely prescribed for depression in Europe and sold as a dietary supplement in the United States, compared to sertraline (Zoloft) in a mouse model of PTSD. Thirty-six mice were tested for baseline ASR, then they were exposed to rats in a predator exposure paradigm known to induce PTSD-like symptoms. Mice were randomly divided into three groups for treatment (control, sertraline, SJW), and ASR was retested one week later. One-way ANOVAs found no significant group differences in ASR amplitude at baseline but a significant effect of Treatment Group after predator exposure, F(2, 33) = 5.645, p = .008, n2 = .225, when SJW-treated mice had ASR amplitudes that were significantly lower than sertraline-treated mice (by 27%) and controls (by 26%). Fecal boli counts showed a similar pattern, with lowest counts in SJW-treated mice. These results suggest SJW could be considered for studies of PTSD treatment in humans as well.
Be well!
JP