Menstrual Cramp Alternatives
May 4, 2011 Written by JP [Font too small?]The concept of connectedness is a guiding principle in the holistic management of dis-ease. On an individual basis this may present itself in how symptoms are viewed. For instance, if you have trouble with indigestion, a holistic physician may consider any number of causes including a bacterial infection, how well you chew, psychological stressors and your food selection. In other words, a symptom is viewed within the context of the whole body and, even, your thought processes. From a more global perspective, connectedness extends to how an individual’s well being impacts those around them. Dysmenorrhea is a prime example of how an imbalance in the body and mind can cause discomfort and pain to those directly and indirectly affected by it.

Dysmenorrhea is the medical term used to describe the mild to severe symptoms that accompany a woman’s menstrual cycle. In some instances, dysmenorrhic manifestations are severe enough to disrupt typical daily activities. It’s no wonder that personal relationships and work performance can be disrupted when you consider the symptoms involved: abdominal cramping and pain that sometimes radiates down the back and legs, dizziness, intestinal issues and sweating.
According to the prestigious Mayo Clinic, the root cause of most painful periods is an elevated concentration of prostaglandins – a variety of “hormone-like substances involved in pain and inflammation” which provoke uterine contractions. The contractions are believed to reduce blood flow, nutrients and oxygen supply to the uterus which results in pain that can be compared to that felt in the heart region during an episode of angina. (1)
There are a number of promising natural interventions that may reduce the likelihood and severity of dysmenorrhea. However it’s a good idea to first rule out any potentially confounding medical issues that could be involved including endometriosis and uterine fibroids. This is an example of why it’s always a good idea to establish a diagnosis even if you plan to approach the symptoms using natural means.
Acupressure vs. Dysmenorrhea: The simple application of pressure to key “acupoints” on the body has been shown to reduce the severity of dysmenorrhea over the long term. In the latest trial, applying acupressure to the Taichong point lead to meaningful improvement in symptoms in a group of 194 female students. A placebo acupoint was used to establish whether the benefits were the result of a genuine therapeutic reaction. This was, in fact, confirmed while following the study participants over a 4 month period. Other acupoints, such as the SP6 point, have also shown profound effects in relation to anxiety and distress associated with dysmenorrhea. (2,3,4)
Fish Oil vs. Dysmenorrhea: Several studies have determined that supplementation with omega-3 fatty acids is an effective and safe way to diminish menstrual discomfort of the body and mind. The latest trial, presented in the April 2010 issue of the Eastern Mediterranean Health Journal reports that a daily dose of 205 mg of DHA and 550 mg of EPA, fatty acids derived from fish, significantly lowered pain scores in a group of 36 young women. The placebo controlled trial also found that this resulted in the use of fewer anti-inflammatory medications. Previous interventions using fish oil and krill oil, another source of omega-3 fatty acids, have similarly demonstrated positive outcomes that have even extended to some of the “emotional symptoms of premenstrual syndrome”. (5,6,7)
Yoga vs. Dysmenorrhea: The practice of yoga may seem complicated and intimidating to some. However, a new study in the Journal of Pediatric and Adolescent Gynecology reveals that working on three basic yoga poses may be enough to address menstrual pain naturally. The specific exercises involved are the cat, cobra and fish poses. A Visual Analog Scale for Pain was used to determine the efficacy of the three poses vs. a control group over the course of three menstrual cycles. According to the authors of the trial, “there was a significant difference in the pain intensity and pain duration in the experimental (yoga) group”. They went on to describe the three yoga poses as a “safe and simple treatment for primary dysmenorrhea”. The proposed mechanism by which yoga influences menstrual symptoms is by moderating the inflammatory response to stressful situations. (8,9,10)
Acupuncture Reduces Pain Medication Use in Patients with Dysmenorrhea
Source: Evid Based Complement Alternat Med. 2008 June; 5(2): 227–230. (link)
There isn’t a strong conviction in the medical community that diet directly influences dysmenorrhea. The best information currently available indicates that several dietary factors may contribute to the incidence and magnitude of menstrual symptoms. Based on my search of the scientific literature, I’ve discovered that the following dietary components, foods and practices may afford a protective affect: a) avoiding gluten; b) eating breakfast daily and; c) including plenty of dairy products, eggs, fish, fiber, fruit and vegetables in your diet. The role that dietary fat plays in dysmenorrhea remains unclear. To my mind, the optimal approach is to limit intake of unhealthy fats (trans fats and most vegetable oils) and replace them with consumption of healthier fats including avocados, fish and olive oil. Balancing the omega-3/omega-6 ratio is known to lower systemic inflammation which would reasonably benefit those with menstrual woes. (11,12,13,14,15,16,17)
At the core of many natural healing regimens is an individualized, nutrient-dense, whole food diet. Adopting the provisional guidelines listed above is good start. But beyond that, I think it would be wise to emphasize foods that are bountiful in select nutrients such as magnesium, thiamine (Vitamin B1) and Vitamin E. A high-potency multivitamin/mineral formula can go a long way to help achieve the therapeutic dosages found to be of value in clinical trials involving those living with dysmenorrhea. Combining mind-body approaches such as acupressure and yoga with nutritional strategies may allow many women to overcome the dread of their monthly cycle. I hope that any of my female readers to whom this applies to will take the above information to heart. And for my male readership, you too can pass this information along to anyone you know that may benefit from it. Helping each other find true wellness is the holistic way. To that extent, we can all be holistic healers.(18,19,20,21,22,23,24)
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
Be well!
JP
Tags: Acupressure, Fish Oil, Yoga
Posted in Alternative Therapies, Nutritional Supplements, Women's Health

May 4th, 2011 at 8:45 pm
I always just went to my library and smoked a cigar.
May 4th, 2011 at 11:04 pm
Ah yes, I’ve heard of such a strategy. 🙂
Be wel1!
JP
May 5th, 2011 at 12:44 pm
Hi JP ☺
i don’t know why and how but green tea esp. matcha tea helps like a wonder drug aganist all menstrual cramps, migraine etc. ..best thing ever, highly recommendet! Maybe it’s the l-theanin, not sure, but it works, always ☺
Nina K.
May 9th, 2011 at 10:48 pm
Nina,
Interesting! And certainly worth a try. Just a theory, but green tea may possibly alter sex hormone binding globulin levels?
http://www.ncbi.nlm.nih.gov/pubmed/9507508
Thanks for sharing your success with us. I hope others find the same to be true!
Be well!
JP
May 12th, 2011 at 7:11 pm
Hi JP! Thanks for this fabulous article. I have edometriosis and am all for food being my medicine: I’m on fish oil and a wheat-free diet. I don’t eat red meat either. Was interesting to see that dairy was helpful for dysmenorrhoea – do know much about dairy and endo? I’ll do a lit search anyway, but just wanted to know if you are aware of anything.
Thanks again,
Lesh
May 15th, 2011 at 12:52 pm
Thank you, Lesh. Dairy *may* have a slight inverse association with endometriosis as well:
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=7978235
http://humrep.oxfordjournals.org/content/19/8/1755.long
Be well!
JP
May 27th, 2011 at 2:30 pm
Licorice tea works great.
February 28th, 2015 at 12:32 am
Update: Lavender oil massage reduces menstrual pain …
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4325408/
Iran J Nurs Midwifery Res. 2015 Jan-Feb;20(1):156-60.
The effect of aromatherapy massage with lavender oil on severity of primary dysmenorrhea in Arsanjan students.
BACKGROUND: Presently, using complementary therapy such as lavender oil has specific application in medicine. The purpose of this study was to investigate the effect of aromatherapy massage on the severity of primary dysmenorrhea in nursing and midwifery students of Islamic Azad University of Arsanjan, Iran.
MATERIALS AND METHODS: This study was performed using clinical trial method on 80 eligible students whose level of pain was measured by visual analogue scale (VAS) before the intervention. Each participant, in the first days of menstruation, randomly received two types of massage with lavender and placebo oil in two consecutive cycles of menstruation. Their level of pain was measured before and 30 min after the intervention. In this study, each group was considered as their self-control group in the next cycle. The data were analyzed by SPSS software.
RESULTS: A significant decrease in VAS score after lavender massage was detected in comparison with placebo massage. There was a statistically significant difference between VAS scores after and before placebo massage. In addition, statistically the effect of lavender massage on the severity of primary dysmenorrhea was higher than that of placebo massage (P < 0.001). CONCLUSIONS: Findings of this study showed that lavender oil massage decreases primary dysmenorrhea and it can be used as an effective herbal drug. Be well! JP
April 12th, 2015 at 10:56 pm
Update 04/12/15:
Complementary Therapies in Clinical Practice – Published Online: April 03, 2015
Effects of Boron supplementation on the severity and duration of pain in primary dysmenorrhea
Background: Primary dysmenorrhea refers to painful menstrual cramps without pelvic pathology. The condition is highly prevalent among women and exerts negative effects on their quality of life. Considering the evidence for anti-inflammatory properties of Boron, the present study aimed to determine the effects of Boron supplementation on the severity and duration of menstrual pain in female university students.
Methods: This triple-blind randomized clinical trial study recruited 113 university students. The participants were matched for the severity and duration of dysmenorrhea and randomly allocated into the case and control groups (n = 58 and 55, respectively). The case group consumed 10 mg/day Boron from two days before the menstrual flow until its third day. The control group received placebo capsules (similar to those distributed among the cases). All subjects were asked to take the capsules for two consecutive menstrual cycles. Pain severity (measured on a visual analogue scale) and duration (in hours) were measured at baseline and during the two cycles.
Results: The two groups had no significant differences in the severity and duration of pain at baseline. After the intervention, however, the severity and duration of pain were significantly lower in the case group than in the control group (P<0.05).
Conclusion: Based on our findings, Boron supplementation can reduce the severity and duration of menstrual pain through exerting anti-inflammatory effects. In order to clarify the effects of Boron on dysmenorrhea, future studies are required to measure the levels of hormones and inflammatory biomarkers.
Be well!
JP
July 20th, 2015 at 6:51 pm
Updated 07/20/15:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437117/
J Clin Diagn Res. 2015 Apr;9(4):QC04-7.
Comparative effect of cinnamon and Ibuprofen for treatment of primary dysmenorrhea: a randomized double-blind clinical trial.
BACKGROUND AND AIMS: Primary dysmenorrheal has a negative impact on women’s quality of life. The purpose of this study was to compare the effect of Cinnamon and Ibuprofen for treatment of primary dysmenorrheal in a sample of Iranian female college students from Ilam University of Medical Sciences (western Iran).
MATERIALS AND METHODS: In a randomized, double-blind trial, out of 114, control group received placebo (empty capsules contain starch, TDS, n= 38) a test group received Ibuprofen (capsule containing 400mg Ibuprofen, TDS, n=38), or another test group received Cinnamon (capsule containing 420 mg Cinnamon, TDS, n= 38) in 24 h. To determine severity of pain, we used the VAS scale. Pain intensity and duration of pain were monitored in the group during first 72 h of cycle.
RESULTS: The mean pain severity score and mean duration of pain in Ibuprofen and Cinnamon were less than placebo group respectively (p< 0.001). Of 4 hours after the intervention there were no statistically significant differences between the Cinnamon and placebo group (p> 0.05). Of eight hours after the intervention, the mean pain severity in the cinnamon group was significantly lower than placebo group (p< 0.001). At various time intervals the mean pain severity in the Ibuprofen group were significantly less than Cinnamon and placebo groups (p< 0.001). CONCLUSION: Cinnamon compared with placebo significantly reduced the severity and duration of pain during menstruation, but this effect was lower compared with Ibuprofen. Cinnamon can be regarded as a safe and effective treatment for primary dysmenorrhea. More researches are recommended to study the efficacy of Cinnamon on reducing menstrual bleeding. Be well! JP
July 20th, 2015 at 6:55 pm
Updated 07/20/15:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4443385/
Iran Red Crescent Med J. 2015 Apr 22;17(4):e27032.
The effect of cinnamon on menstrual bleeding and systemic symptoms with primary dysmenorrhea.
BACKGROUND: Primary dysmenorrhea with interferes in daily activities can have adverse effects on quality of life of women.
OBJECTIVES: Regarding the use of herbal medicine, the aim of this study was to assess the effect of cinnamon on primary dysmenorrhea in a sample of Iranian female college students from Ilam University of Medical Sciences (west of Iran) during 2013-2014.
PATIENTS AND METHODS: In a randomized double-blind trial, 76 female student received placebo (n = 38, capsules containing starch, three times a day (TDS)) or cinnamon (n = 38, capsules containing 420 mg cinnamon, TDS) in 24 hours. Visual analogue scale (VAS) was used to determine the severity of pain and nausea. Vomiting and menstrual bleeding were assessed by counting the number of saturated pads. The parameters were recorded in the group during the first 72 hours of the cycle.
RESULTS: The mean amount of menstrual bleeding in the cinnamon group was significantly lower than the placebo group (P < 0.05 and P < 0.001, respectively). The mean pain severity score in the cinnamon group was less than the placebo group at various intervals (4.1 ± 0.5 vs. 6.1 ± 0.4 at 24 hours, 3.2 ± 0.6 vs. 6.1 ± 0.4 at 48 hours, and 1.8 ± 0.4 vs. 4.0 ± 0.3 at 72 hours, respectively) (P < 0.001). The mean severity of nausea and the frequencies of vomiting significantly decreased in the cinnamon group compared with the placebo group at various intervals (P < 0.001, P < 0.05). CONCLUSIONS: Regarding the significant effect of cinnamon on reduction of pain, menstrual bleeding, nausea and vomiting with primary dysmenorrhea without side effects, it can be regarded as a safe and effective treatment for dysmenorrhea in young women. Be well! JP
July 26th, 2015 at 9:08 pm
Updated 07/26/15:
http://www.ncbi.nlm.nih.gov/pubmed/26177393
Pain Med. 2015 Jul 14.
Efficacy of Ginger for Alleviating the Symptoms of Primary Dysmenorrhea: A Systematic Review and Meta-analysis of Randomized Clinical Trials.
OBJECTIVE: There has been no attempt to date to synthesize the available evidence for the efficacy of ginger for treating primary dysmenorrhea. This systematic review evaluates the current evidence for the effectiveness of ginger for treating primary dysmenorrhea.
METHODS: Literature searches were conducted using 12 electronic databases including PubMed, EMBASE, Cochrane Library, Korean databases, Chinese medical databases, and Indian scientific database. Search terms used were: “ginger” or “Zingiber officinale” and “dysmenorrhea” and “pain.” Studies using ginger as a treatment of primary dysmenorrhea were considered for inclusion. The major outcome of primary dysmenorrhea was assessed using a pain visual analogue score (PVAS).
RESULTS: Initial searches yielded 29 articles. Of these original results, seven met specific selection criteria. Four of the RCTs compared the therapeutic efficacy of ginger with a placebo during the first 3-4 days of the menstrual cycle and were included in the meta analysis. The meta-analysis of these data showed a significant effect of ginger in reducing PVAS in subjects having primary dysmenorrhea (risk ratio, -1.85; 95% CI of -2.87, -0.84, P = 0.0003). Six RCTs out of 7 exhibited low to moderate of risk of bias.
CONCLUSION: Collectively these RCTs provide suggestive evidence for the effectiveness of 750-2000 mg ginger powder during the first 3-4 days of menstrual cycle for primary dysmenorrhea.
Be well!
JP
August 18th, 2015 at 8:22 pm
Updated 08/18/15:
http://www.jpagonline.org/article/S1083-3188%2815%2900033-9/abstract
J Pediatr Adolesc Gynecol. 2015 Mar 5.
Comparison of the Effect of Massage Therapy and Isometric Exercises on Primary Dysmenorrhea: A Randomized Controlled Clinical Trial.
STUDY OBJECTIVE: Dysmenorrhea is the most common cyclic pelvic pain, and it affects the quality of life of many women. We sought to compare the effects of massage and isometric exercises on primary dysmenorrhea.
DESIGN, SETTING, AND PARTICIPANTS: We conducted a randomized controlled trial at the dormitories of Shiraz University among 102 students with primary dysmenorrheal.
INTERVENTIONS: The student groups were randomly divided into massage, isometric exercises, and control groups. The first group received 2 consecutive cycles of effleurage massage with lavender oil. The second group had 8 weeks of isometric exercises. No intervention was performed for the control group.
MAIN OUTCOME MEASUREMENTS: Pain intensity was measured and recorded by using a visual analog scale. In addition, the duration of pain was measured in hours, and Spielberger’s questionnaire was used to measure the anxiety level.
RESULTS: Pain intensity had significantly reduced in the massage and exercises groups; the reduction was more significant in the massage group (P < .001). The results revealed a significant difference among the 3 groups in regard to the mean duration of pain after the third cycle (P = .006). However, no significant difference was found among the 3 groups concerning the mean level of anxiety. The results of intragroup comparisons only showed a significant reduction of anxiety level in the massage group after the third cycle (P = .017). CONCLUSION: Based on the present findings, it seems that massage therapy and isometric exercises were effective in reducing some symptoms of dysmenorrhea. Be well! JP
September 10th, 2015 at 7:01 pm
Updated 09/10/15:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4539461/
Evid Based Complement Alternat Med. 2015;2015:735690.
Efficacy of Acupuncture versus Combined Oral Contraceptive Pill in Treatment of Moderate-to-Severe Dysmenorrhea: A Randomized Controlled Trial.
This open-label randomized controlled trial was designed to compare the efficacy of acupuncture and combined oral contraceptive (COC) pill in treating moderate-to-severe primary dysmenorrhea. Fifty-two participants were randomly assigned to receive either acupuncture (n = 27) or COC (n = 25) for three menstrual cycles. Mefenamic acid was prescribed as a recue analgesic drug with both groups. The statistical approach used for efficacy and safety assessments was intention-to-treat analysis. By the end of the study, both treatments had resulted in significant improvement over baselines in all outcomes, that is, maximal dysmenorrhea pain scores, days suffering from dysmenorrhea, amount of rescue analgesic used, and quality of life assessed by SF-36 questionnaire. Over the three treatment cycles, COC caused greater reduction in maximal pain scores than acupuncture, while improvements in the remaining outcomes were comparable. Responders were defined as participants whose maximal dysmenorrhea pain scores decreased at least 33% below their baseline. Response rates following both interventions at the end of the study were not statistically different. Acupuncture commonly caused minimal local side effects but did not cause any hormone-related side effects as did COC. In conclusion, acupuncture is an alternative option for relieving dysmenorrhea, especially when COC is not a favorable choice.
Be well!
JP
June 18th, 2016 at 4:11 pm
Updated 06/18/16:
http://www.ncbi.nlm.nih.gov/pubmed/27315239
J Altern Complement Med. 2016 Jun 17.
Effects of a Yoga Program on Menstrual Cramps and Menstrual Distress in Undergraduate Students with Primary Dysmenorrhea: A Single-Blind, Randomized Controlled Trial.
OBJECTIVES: To investigate the effects of a yoga program on menstrual cramps and menstrual distress in undergraduate students with primary dysmenorrhea.
DESIGN: Single-blind, randomized controlled trial.
PARTICIPANTS: 40 randomly selected undergraduate nursing students, with 20 each assigned to an exercise or a control group.
INTERVENTION: The participants engaged in a yoga program for 60 minutes once a week for 12 weeks. The program consisted of physical exercise combined with relaxation and meditation.
OUTCOME MEASURES: Menstrual cramps and menstrual distress levels were measured by using the Visual Analogue Scale for Pain and the Menstrual Distress Questionnaire, respectively. Data were analyzed by using the Kolmogorov-Smirnov and Shapiro-Wilk normality tests, t-test, chi-square test, logistic regression analysis, and multivariate analysis of variance (SPSS program).
RESULTS: Menstrual pain intensity (group difference, -0.94; 95% confidence interval [CI], -1.47 to -0.42; p = 0.001) and menstrual distress (group difference, -1.13; 95% CI, -1.43 to -0.82; p < 0.0001) scores decreased significantly in the experimental group compared with the control group. CONCLUSIONS: These findings indicate that yoga interventions may reduce menstrual cramps and menstrual distress in female undergraduate students with primary dysmenorrhea. Be well! JP
August 22nd, 2016 at 6:27 pm
Updated 08/22/16:
http://onlinelibrary.wiley.com/wol1/doi/10.1111/jnu.12238/abstract
J Nurs Scholarsh. 2016 Aug 19.
Effects of Auricular Acupressure Therapy on Primary Dysmenorrhea for Female High School Students in South Korea
PURPOSE: To examine the effect of auricular acupressure therapy on primary dysmenorrhea among female high school students in South Korea.
DESIGN: A randomized controlled trial was employed.
METHODS: The study sample consisted of 91 female high school students, with 45 participants in the experimental group and 46 in the control group in two regions of South Korea. The average age of the participants was 16.7 years, and the average age of menarche was 12.2 years. Auricular acupressure therapy including an auricular acupressure needle on skin paper tape was applied on an ear for 3 days during periods of extreme primary dysmenorrhea. The acupoint names were Jagung, Sinmun, Gyogam, and Naebunbi. For the placebo control group, only the skin paper tape without an auricular acupressure needle was applied on the same acupoints. Measures used were the Menstrual Distress Questionnaire to assess primary dysmenorrhea, and the visual analog scale to assess abdominal and back pain of participants.
FINDINGS: There were significant differences on abdominal pain (t = 24.594, p < .001), back pain (t = 22.661, p < .001), and primary dysmenorrhea (t = 32.187, p < .001) between the two groups. Auricular acupressure therapy decreased abdominal pain, back pain, and primary dysmenorrhea of female high school students in South Korea. CONCLUSIONS: Auricular acupressure therapy was an effective intervention for alleviating abdominal pain, back pain, and primary dysmenorrhea of female high school students in South Korea. For feasibility of the auricular acupressure therapy in practice, it is needed to train and learn the exact positions of acupoints in ear. CLINICAL RELEVANCE: Health providers should consider providing auricular acupressure therapy as an alternative method for reducing abdominal and back pain, and primary dysmenorrhea in female high school students in South Korea. Be well! JP
September 10th, 2016 at 7:21 pm
Updated 09/10/16:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979258/
Iran J Nurs Midwifery Res. 2016 Jul-Aug;21(4):363-7.
Evaluation of mint efficacy regarding dysmenorrhea in comparison with mefenamic acid: A double blinded randomized crossover study.
BACKGROUND: Menthol is the most important active material in mint and different mechanisms have been suggested for the way mint functions, most of which emphasize its analgesic effect owing to the presence of a group of temporary protein receptors. This study investigates the efficacy of peppermint capsule in the treatment of primary dysmenorrhea, in comparison with Mefenamic Acid and placebo.
MATERIALS AND METHODS: This was a prospective, double-blinded, crossover study and was conducted on 127 girl students studying in Hamadan University of Medical Sciences who had experienced primary dysmenorrhea. Each participant was asked to take one of the drugs including Mefenamic Acid and Mint, starting from the first menstruation for 3 days. At the end of each period, a questionnaire was used to gather information; through the volunteer herself, pain intensity was recorded according to visual analog scale (VAS), duration of pain according to COX questionnaire, and bleeding amount according to pictorial blood loss assessment chart (PBAC) chart (Hygham).
RESULTS: Average pain intensity and duration of pain were significantly lower after intake of Mefenamic Acid and Mint (P < 0.05). Average bleeding was significantly lower in those taking Mefenamic Acid capsule than in those taking peppermint extract (P < 0.05). Nausea and diarrhea were lower in the mint group than in Mefenamic Acid group. But analgesic usage was lower in Mefenamic Acid group than in peppermint group (P < 0.05). CONCLUSIONS: While the bleeding amount did not significantly change, pain and its severity and all the clinical signs and symptoms decreased after taking peppermint extract. Because the side effect of herbal drugs is lower than other medicinal drugs, using mint is advised for treating dysmenorrhea symptoms. Be well! JP
July 7th, 2017 at 1:12 pm
Updated 07/07/17:
https://www.ncbi.nlm.nih.gov/pubmed/28659234
J Integr Med. 2017 Jul;15(4):295-301.
Use of ginger versus stretching exercises for the treatment of primary dysmenorrhea: a randomized controlled trial.
BACKGROUND: Dysmenorrhea is a common gynecologic problem. In some cases, non-medical treatments are considered to be more effective, with fewer side effects. Ginger and exercise are alternative treatments for dysmenorrhea, but in the present study they were not combined.
OBJECTIVE: In this study, the effects of ginger and exercise on primary dysmenorrhea were compared.
DESIGN, SETTING, PARTICIPANTS AND INTERVENTIONS: This randomized controlled trial was performed in Mazandaran University of Medical Sciences, Iran. Two groups of female students were recruited by simple random allocation. In each group, 61 students with moderate to severe primary dysmenorrhea with regular menstrual cycles and without a history of regular exercise were assessed. The ginger group received 250 mg ginger capsules from the onset of menstruation. In the exercise group, belly and pelvic stretching exercises were performed for 10 min, 3 times per week.
MAIN OUTCOME MEASURES: Intensity of pain was assessed according to a visual analogue scale after the first and the second month.
RESULTS: Exercise was significantly more effective than ginger for pain relief (31.57 ± 16.03 vs 38.19 ± 20.47, P = 0.02), severity of dysmenorrhea (63.9% vs 44.3% mild dysmenorrhea, P = 0.02) and decrease in menstrual duration (6.08 ± 1.22 vs 6.67 ± 1.24, P = 0.006), in the second cycle.
CONCLUSION: Stretching exercises, as a safe and low-cost treatment, are more effective than ginger for pain relief in primary dysmenorrhea.
Be well!
JP
September 18th, 2017 at 11:55 am
Updated 09/18/17:
https://www.ncbi.nlm.nih.gov/pubmed/28917360
Complement Ther Med. 2017 Oct;34:10-15.
A randomized controlled clinical trial evaluating quality of life when using a simple acupressure protocol in women with primary dysmenorrhea.
OBJECTIVE: To evaluate a simple acupressure protocol in LIV3 and LI4 acupoints in women with primary dysmenorrhea.
METHODS: This paper reports a randomized, single blinded clinical trial. 90 young women with dysmenorrhea were recruited to three groups to receive 20min acupressure every day in either LIV3 or LI4, or placebo points. Acupressure was timed five days before menstruation for three successive menstrual cycles. On menstruation, each participant completed the Wong Baker faces pain scale, and the quality of life short form -12 (QOL SF-12).
RESULTS: Intensity and duration of pain between the three groups in the second and third cycles during the intervention (p<0.05) differed significantly. Significant differences were seen in all domains of QOL except for mental health (p=0.4), general health (p=0.7) and mental subscale component (p=0.12) in the second cycle, and mental health (p=0.9), and mental subscale component (p=0.14) in the third cycle.
CONCLUSION: Performing the simple acupressure protocol is an effective method to decrease the intensity and duration of dysmenorrhea, and improve the QOL.
Be well!
JP
October 19th, 2017 at 9:02 pm
Updated 10/19/17:
https://www.ncbi.nlm.nih.gov/pubmed/29037637
J Bodyw Mov Ther. 2017 Oct;21(4):840-846.
Effect of yoga on the menstrual pain, physical fitness, and quality of life of young women with primary dysmenorrhea.
The aim of the present study was to investigate effect of specially designed yoga program on the menstrual pain, physical fitness, and quality of life (QOL) of non-athlete women with primary dysmenorrhea (PD) aged 18-22 years. Thirty-four volunteers were randomly assigned into control and yoga groups. Menstrual pain, physical fitness, and QOL were evaluated at baseline and at the end of the 12-week study period. The yoga group was asked to practice yoga for 30 min per day, twice a week, for 12 weeks at home, while the control group did not receive any form of exercise over the study period. There were significant improve in menstrual pain, physical fitness, and QOL in the yoga group more than the control group. Therefore, this specially designed yoga program may be a possible complementary treatment for PD.
Be well!
JP
November 22nd, 2017 at 2:17 pm
Updated 11/21/17:
http://www.ajog.org/article/S0002-9378(17)32335-9/pdf
Am J Obstet Gynecol. 2017 Nov 15.
Effectiveness of app-based self-acupressure for women with menstrual pain compared to usual care: A randomized pragmatic trial.
BACKGROUND: Primary dysmenorrhea is common among women of reproductive age. Non-steroidal anti-inflammatory drugs and oral contraceptives are effective treatments, although the failure rate is around 20-25%. Therefore additional evidence-based treatments are needed. In recent years, the use of smartphone applications (apps) has increased rapidly and may support individuals in self-management strategies.
OBJECTIVE: We aimed to investigate the effectiveness of app-based self-acupressure in women with menstrual pain.
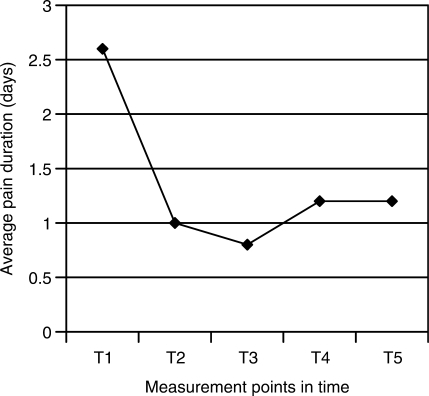
MATERIALS AND METHODS: A two-armed randomized pragmatic trial was conducted from December 2012 to April 2015 with recruitment until August 2014 in Berlin, Germany, among women aged 18-34 years with self reported cramping pain ≥6 on a numeric rating scale (NRS) for the worst pain intensity during the previous menstruation. After randomization women performed either app-based self-acupressure (n=111) or followed usual care only (n=110) for six consecutive menstruation cycles. The primary outcome was the mean pain intensity (NRS 0-10) on the days with pain during the third menstruation. Secondary outcomes included worst pain intensity during menstruation, duration of pain, 50% responder rates (reduction of mean pain by at least 50%), medication intake, sick leave days and body efficacy expectation assessed at the 1st, 2nd, 3rd, and 6th menstruation cycle.
RESULTS: We included 221 women (mean age 24.0 (sd 3.6) years). The mean pain intensity difference during the third menstruation was statistically significant in favor for acupressure (acupressure: 4.4 95% CI [4.0; 4.7]; usual care 5.0 [4.6; 5.3]; mean difference -0.6 [-1.2; -0.1], p=0.026). At the sixth cycle, the mean difference between the groups -1.4 [-2.0; -0.8] (p<0.001) reached clinical relevance. At the third and sixth menstruation cycle, responder rate was 37% and 58% respectively in the acupressure group in contrast to 23% and 24% in the usual care group. Moreover, the worst pain intensity (group difference -0.6 [-1.2; -0.02] and -1.4 [-2.0; -0.7]), the number of days with pain (-0.4 [-0.9; -0.01] and -1.2 [-1.6; -0.7]) and the proportion of women with pain medication at the third and sixth menstruation cycle (odd ratio 0.5 [0.3; 0.9] and 0.3 [0.2; 0.5]) was lower in the acupressure group. At the third cycle hormonal contraceptive use was more common in the usual care group than in the acupressure group (odds ratio 0.5 [0.3;0.97]), but not statistically significant different at the sixth cycle (odds ratio 0.6 [0.3;1.1]). The number of sick leave days and body efficacy expectation (self-efficacy scale) did not differ between groups. On a scale from 0-6, mean satisfaction with the intervention at the third cycle was 3.7 (sd 1.3), recommendation of the intervention to others 4.3 (1.5), appropriateness of acupressure for menstrual pain 3.9 (1.4), and application of acupressure for other pain 4.3 (1.5). The intervention was safe and after the sixth cycle two third of the women (67.6%) still applied acupressure on all days with pain.
CONCLUSION: Smartphone app delivered self-acupressure resulted in a reduction of menstrual pain compared to usual care only. Effects were increasing over time and adherence was good. Future trials should include comparisons to other active treatment options.
Be well!
JP
February 16th, 2018 at 3:24 pm
Updated 2/16/18:
http://www.tandfonline.com/doi/abs/10.1080/09513590.2017.1423466?journalCode=igye20
Gynecol Endocrinol. 2018 Feb 15:1-5.
High dose vitamin D supplementation can improve menstrual problems, dysmenorrhea, and premenstrual syndrome in adolescents.
Vitamin D has a crucial role in female reproduction, possibly through its effects on calcium homeostasis, cyclic sex steroid hormone fluctuations, or neurotransmitter function. We have assessed the effects of vitamin D supplementation on dysmenorrhea and premenstrual syndrome (PMS) in adolescents. In this study, 897 adolescent girls living in Mashhad and Sabzevar, Iran, received nine high-dose vitamin D supplements (as 50,000 IU/week of cholecalciferol) and were followed up over 9 weeks. We evaluated the effect of vitamin D supplementation on individuals in four categories: those with only PMS; individuals with only dysmenorrhea; subjects with both PMS and dysmenorrhea and normal subjects. The prevalence of PMS after the intervention fell from 14.9% to 4.8% (p < .001). Similar results were also found for the prevalence of subjects with dysmenorrhea (35.9% reduced to 32.4%), and in subjects with both PMS and dysmenorrhea (32.7% reduced 25.7%). Vitamin D supplementation was associated with a reduction in the incidence of several symptoms of PMS such as backache and tendency to cry easily as well as decrement in pain severity of dysmenorrhea (p < .05). High dose vitamin D supplementation can reduce the prevalence of PMS and dysmenorrhea as well as has positive effects on the physical and psychological symptoms of PMS. Be well! JP
December 17th, 2018 at 7:03 pm
Updated 12/17/18:
https://www.ncbi.nlm.nih.gov/pubmed/30545531
Taiwan J Obstet Gynecol. 2018 Dec;57(6):806-809.
Effect of Ginger and Novafen on menstrual pain: A cross-over trial.
OBJECTIVE: Menstrual pain is a periodic pain which happens during the days of menses. The menstrual disturbances as a health problem among young girls affect not only reproductive, but also psychical health and quality of life. This study was done with the goal of comparing the effect of Ginger and Novafen on the menstrual pain.
MATERIALS AND METHODS: This crossover clinical trial study was done in Iran on 168 single girl students 18-26 years old in Babol University of Medical Sciences with primary menstrual pain. The participants were randomly allocated to two groups receiving the drugs Novafen and Ginger. At the beginning of pain, in the two groups 200 mg capsule was given every 6 h for two serial cycles. Pain severity was measured by the visual scale before treatment, 1 h after consuming the drug (for 24 h) and 48 h after the onset of drug.
RESULTS: The mean age of participants was 21.83 ± 2.07 years. It has been reported that the intensity of pain from dysmenorrhea decreased in the Novafen and Ginger groups. Before treatment, the average pain intensity in Novafen and Ginger users were 7.12 ± 2.32 and 7.60 ± 1.84, respectively and after treatment pain intensity decreased to 3.10 ± 2.69 and 2.97 ± 2.69, respectively. Differences between two groups each time showed no statistical significance (p > 0.05).
CONCLUSION: Both drugs reduced menstrual pain. Ginger as well as Novafen is effective in relieving pain in girls with primary dysmenorrhea . Therefore, treatment with natural herbal medicine, non-synthetic drug, to reduce primary dysmenorrhea is recommended.
Be well!
JP