Female Libido Support Part One
June 24, 2015 Written by JP [Font too small?]Men with erectile dysfunction (ED) have access to several medical options to improve sexual function. Popular medications, including Cialis, Viagra and testosterone replacement top the list of medically-approved, male performance aids. What isn’t discussed as much is that many women also deal with a related condition known as hypoactive sexual desire disorder (HSDD). Obviously, the mechanism involved is somewhat different. Nevertheless, the end result is similar: compromised sexual desire and enjoyment. This may soon change. Flibanserin, a medication intended to treat premenopausal HSDD, is on the brink of FDA approval. If approved, it is likely to become as big a blockbuster as its male counterparts.
A 2008 study appearing in JAMA Internal Medicine reports that HSDD is quite prevalent indeed. According to an analysis of over 2,200 women, approximately 27% of premenopausual and 52% of postmenopausual women deal with low sexual desire. Flibanserin aims to address this widespread problem by altering brain chemistry. Specifically, it “improves sexual functioning by enhancing downstream release of dopamine and norepinephrine while reducing serotonin release in the brain circuits that mediate symptoms of reduced sexual interest and desire”. However, some FDA reviewers have expressed concern about the limited amount of clinical research and documented side effects such as dizziness, fatigue, headaches, nausea and sleep disturbance.
Since at least part of the issue with HSDD involves the brain, there are several mind-body techniques that may provide an alternative to flibanserin. The upside to these remedies is that they’re virtually free of adverse reactions and tend to promote overall wellness as a bonus.
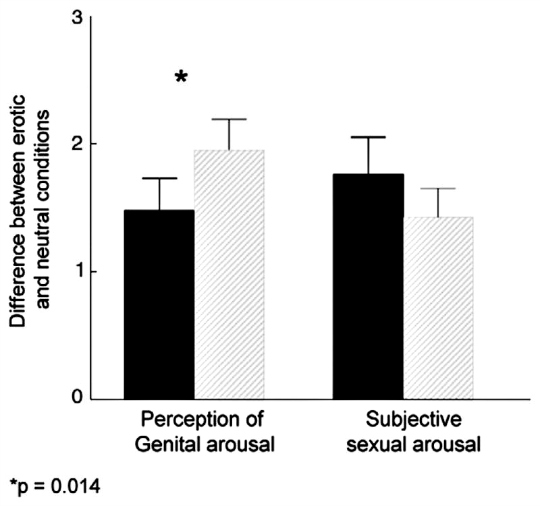
Mindfulness and Sexual Intimacy – Mindfulness meditation have been shown to improve various aspects of sexual intimacy. One study reports that mindfulness training enhanced physical response to sexual stimuli and lowered psychological factors that negatively influence sexuality such as anxiety, depression and self judgment. Also, couples and group mindfulness education have been found to promote sexual desire, while minimizing feelings of distress. Of note, the couples’ work lead to unique benefits for both partners – less depression in the women and greater well-being in the men.
“Pilates for Better Sex” – A first of its kind trial, appearing in the March 2015 edition of the Journal of Sex & Marital Therapy, discovered that 12 weeks of Pilates practice not only improved the Female Sexual Function Index in 34 premenopausal women, but also reduced depressive symptoms.
Yoga and Sexual Function – Two studies have concluded that 12 weeks of yoga practice positively influences sexual dysfunction in women of all ages. Various symptoms pertaining to HSDD improved such as: arousal, lubrication, orgasm and satisfaction. Additional data suggest that yoga may support sexual function and health by reducing the impact of hormonal changes associated with menopause.
It’s unclear exactly how mindfulness, Pilates and yoga directly or indirectly influence HSDD. One theory is that all three of these mind-body practices tend to improve heart rate variability (HRV). Emerging research reveals that women with below average HRV are “more likely to report sexual arousal dysfunction and overall sexual dysfunction”. Additionally, mind-body exercises generally alleviate anxious feelings to some degree. According to one trial, reducing anxiety by supplementing with kava root extract significantly increases female sexual drive. I’ll address other supplement options in part two of this column. But, until then, it seems that various means of improving brain chemistry and psychological health may be an important piece of the HSDD puzzle.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Mechanism of Action of Flibanserin, A Multifunctional Serotonin Agonist … (link)
Study 2 – Flibanserin for Female Sexual Dysfunction … (link)
Study 3 – Prevalence of Low Sexual Desire and Hypoactive Sexual Desire Disorder … (link)
Study 4 – Effects of Mindfulness Training on Body Awareness to Sexual Stimuli … (link)
Study 5 – A Mindfulness-Based Group Psychoeducational Intervention Targeting … (link)
Study 6 – Sex-Specific Effects of Mindfulness on Romantic Partners’ Cortisol … (link)
Study 7 – Pilates for Better Sex: Changes in Sexual Functioning in Healthy Turkish … (link)
Study 8 – Effects of Yoga on Sexual Function in Women with Metabolic Syndrome … (link)
Study 9 – Yoga in Female Sexual Functions … (link)
Study 10 – Effect of Yoga Therapy on Physical and Psychological Quality of Life of … (link)
Study 11 – Heart Rate Variability: A Risk Factor for Female Sexual Dysfunction … (link)
Study 12 – Kava for the treatment of generalized anxiety disorder RCT … (link)
Mindfulness Improves Certain HSDD Symptoms
Source: Gynecol Oncol. 2012 May;125(2):320-5. (link)
Tags: Pilates, Sex, Yoga
Posted in Alternative Therapies, Mental Health, Women's Health


June 24th, 2015 at 5:58 pm
Update 06/24/15:
http://www.ctcpjournal.com/article/S1744-3881%2814%2900038-3/abstract
Complement Ther Clin Pract. 2014 Aug;20(3):164-71. doi: 10.1016/j.ctcp.2014.05.002. Epub 2014 Jun 11.
Rusie Dutton traditional Thai exercise promotes health related physical fitness and quality of life in menopausal women.
OBJECTIVE: To examine the effects of “Rusie Dutton” on health and quality of life in menopausal women.
METHOD: Menopausal women (aged 45-59) were recruited and randomly allocated to 2 groups. Rusie Dutton group (n = 24) practiced Rusie Dutton conducted by Wat Pho Thai Traditional Massage School for 13 weeks. The control group (n = 26) was assigned to a waiting list and received no intervention. BW, BMI, restingHR, BP, flexibility, VO2max, and MENQOL including vasomotor, physical, psychosocial and sexual domains were measured at the beginning and the end. A paired-sample t-test and independent sample t-test were used for statistical analysis.
RESULTS: Significant improvement was found in all variables within group (p < .05) in Rusie Dutton group, and a significant difference between groups was found (p < .05) in all variables except BW and BMI. Therefore, it is concluded that the traditional Thai exercise Rusie Dutton can promote health related physical fitness and QOL in menopausal women. Be well! JP
June 24th, 2015 at 5:58 pm
Update 06/24/15:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4106820/
Arq Bras Cardiol. 2013 Dec; 101(6): e107–e108.
Cardiovascular Rehabilitation, Ballroom Dancing and Sexual Dysfunction
The advantage of dancing as compared to conventional exercise methods incorporated to CPMR is mainly due to its characteristic of bringing people closer together, both physically and emotionally. In that context, ballroom dancing can be seen as a strategy to concomitantly treat cardiovascular diseases and sexual dysfunction.
Be well!
JP
June 24th, 2015 at 5:59 pm
Update 06/24/15:
http://www.tandfonline.com/doi/abs/10.1080/713847125?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
J Sex Marital Ther. 2003;29 Suppl 1:33-44.
Randomized, placebo-controlled, double blind, crossover design trial of the efficacy and safety of Zestra for Women in women with and without female sexual arousal disorder.
Zestra for Women is a botanical feminine massage oil formulated to enhance female sexual pleasure and arousal when applied to the vulva. We conducted this randomized, double-blinded, crossover study to evaluate the efficacy and safety of Zestra for Women compared to placebo oil in 10 women with and 10 women without female sexual arousal disorder (FSAD) in conditions of home use in conjunction with sexual activities. Subjects were screened by physical examination, sex therapist interviews, and questionnaires. We randomized qualified subjects to treatment paths and gave them 5 doses of test article and diaries to use at home. At Visit 2, we assessed them by questionnaires and gave them 5 doses of crossover test article and diaries to use at home. At the final visit, we assessed them with questionnaires. We assessed safety by adverse event reports and primary efficacy by responses to a diary question regarding satisfaction with arousal. Secondary efficacy instruments included remaining diary questions, recall-based questionnaires, global assessment questions, and a consumer-testing questionnaire. All 20 subjects completed the study. Three subjects reported single incidences of mild genital burning sensations lasting 5-30 min after use of Zestra for Women. Both normal and FSAD women showed statistically significant improvements, relative to placebo, in level of arousal, level of desire, satisfaction with arousal, genital sensation, ability to have orgasms, and sexual pleasure. Although FSAD women showed greater magnitude of response, the presence of FSAD had no effect on response rates. Zestra for Women was just as effective in women using selective serotonin reuptake inhibitor antidepressants as in women not using antidepressants. Zestra for Women improved sexual function in normal and FSAD women under conditions of home use.
Be well!
JP
June 26th, 2015 at 2:27 pm
Update 06/26/15:
http://onlinelibrary.wiley.com/doi/10.1111/jsm.12830/abstract
J Sex Med. 2015 Apr;12(4):1019-27.
Acupuncture for the treatment of vulvodynia: a randomized wait-list controlled pilot study.
INTRODUCTION: The incidence of vulvodynia in American women has been reported to be between 8.3% and 16%. However, there is no consistently effective standardized treatment for vulvodynia.
AIM: To determine the feasibility and potential effects of using a standardized acupuncture protocol for the treatment of women with vulvodynia.
MAIN OUTCOME MEASURES: The primary outcome was vulvar pain, and sexual function was the secondary outcome. Pain was assessed by the Short-Form McGill Pain Questionnaire, and function was measured by the Female Sexual Function Index (FSFI).
METHODS: Thirty-six women with vulvodynia met inclusion criteria. The women were randomly assigned either to the acupuncture group or to the wait-list control group. The 18 subjects assigned to the acupuncture group received acupuncture two times per week for 5 weeks for a total of 10 sessions.
RESULTS: Reports of vulvar pain and dyspareunia were significantly reduced, whereas changes in the aggregate FSFI scores suggest significant improvement in sexual functioning in those receiving acupuncture vs. those who did not. Acupuncture did not significantly increase sexual desire, sexual arousal, lubrication, ability to orgasm or sexual satisfaction in women with vulvodynia.
CONCLUSION: This was the first randomized controlled pilot study to examine the use of acupuncture for the treatment of vulvodynia. The acupuncture protocol was feasible and in this small sample appeared to reduce vulvar pain and dyspareunia with an increase in overall sexual function for women with vulvodynia. This study should be replicated in a larger double-blinded randomized controlled trial.
Be well!
JP
July 15th, 2015 at 9:36 pm
Updated 07/15/15:
http://www.ncbi.nlm.nih.gov/pubmed/26170587
Int J Yoga. 2015 Jul-Dec;8(2):96-102.
Resting heart rate variability after yogic training and swimming: A prospective randomized comparative trial.
CONTEXT: Resting heart rate variability (HRV) is a measure of the modulation of autonomic nervous system (ANS) at rest. Increased HRV achieved by the exercise is good for the cardiovascular health. However, prospective studies with comparison of the effects of yogic exercises and those of other endurance exercises like walking, running, and swimming on resting HRV are conspicuous by their absence.
AIMS: Study was designed to assess and compare the effects of yogic training and swimming on resting HRV in normal healthy young volunteers.
SETTINGS AND DESIGN: Study was conducted in Department of Physiology in a medical college. Study design was prospective randomized comparative trial.
SUBJECTS AND METHODS: One hundred sedentary volunteers were randomly ascribed to either yoga or swimming group. Baseline recordings of digital electrocardiogram were done for all the subjects in cohorts of 10. After yoga training and swimming for 12 weeks, evaluation for resting HRV was done again.
STATISTICAL ANALYSIS USED: Percentage change for each parameter with yoga and swimming was compared using unpaired t-test for data with normal distribution and using Mann-Whitney U test for data without normal distribution.
RESULTS: Most of the HRV parameters improved statistically significantly by both modalities of exercise. However, some of the HRV parameters showed statistically better improvement with yoga as compared to swimming.
CONCLUSION: Practicing yoga seems to be the mode of exercise with better improvement in autonomic functions as suggested by resting HRV.
Be well!
JP
April 2nd, 2016 at 2:10 pm
Updated 04/02/16:
http://www.ncbi.nlm.nih.gov/pubmed/27033339
Sex Med. 2016 Mar 28.
Acupuncture in Premenopausal Women With Hypoactive Sexual Desire Disorder: A Prospective Cohort Pilot Study.
INTRODUCTION: Female sexual dysfunction affects up to 43% of women in the United States and hypoactive sexual desire disorder (HSDD) is the most common type; however, we lack treatment options showing improvement for this condition.
AIMS: To investigate whether acupuncture therapy could improve HSDD.
METHODS: Premenopausal women with a primary diagnosis of HSDD were included in a single-arm prospective pilot study that was approved by the institutional review board. After providing informed consent, subjects completed validated questionnaires. Participants underwent 25-minute twice-weekly acupuncture sessions for 5 weeks with one certified acupuncturist. Questionnaires were completed again 6 weeks after onset of treatment.
MAIN OUTCOME MEASURES: Based on a statistically significant change in the desire domain of the Female Sexual Function Index from 2.0 (at baseline) to 2.4 (after intervention with a specialist) in our population of patients diagnosed with HSDD, a sample of 13 was determined, with 90% power and α 0.05.
RESULTS: Fifteen women were enrolled and 13 completed the study. Mean age was 36.9 ± 11.4 years. Most were white (n = 9, 60%), heterosexual (n = 15, 100%), and non-smokers (n = 14, 93%). Most were sexually active more than four times per month (n = 8, 53%) and none had a history of sexual abuse (n = 15, 100%). Participants received a mean acupuncture needle application of 17 ± 2 at each session. Sexual function improved after intervention, particularly desire (2.1 ± 0.6 to 3.3 ± 1.2, P < .0001), arousal (P < .0001), lubrication (P = .03), and orgasm (P = .005). CONCLUSION: In this cohort of premenopausal women with HSDD, 5 weeks of acupuncture therapy was associated with significant improvements in sexual function, particularly desire. This supports a role for acupuncture as a therapeutic option for women with low desire. Be well! JP
September 26th, 2018 at 3:27 pm
Updated 09/26/18:
https://onlinelibrary.wiley.com/doi/abs/10.1111/ner.12846
Neuromodulation. 2018 Sep 3.
Transcutaneous Electrical Nerve Stimulation to Improve Female Sexual Dysfunction Symptoms: A Pilot Study.
OBJECTIVES: To perform a pilot study using transcutaneous electrical nerve stimulation (TENS) on the dorsal genital nerve and the posterior tibial nerve for improving symptoms of female sexual dysfunction (FSD) in women without bladder problems. We hypothesize that this therapy will be effective at improving genital arousal deficits.
MATERIALS AND METHODS:
Nine women with general FSD completed the study. Subjects received 12 sessions of transcutaneous dorsal genital nerve stimulation (DGNS; n = 6) or posterior tibial nerve stimulation (PTNS; n = 3). Stimulation was delivered for 30 min at 20 Hz. Sexual functioning was evaluated with the female sexual functioning index (FSFI), and surveys were also given on general health, urological functioning, and the Patients’ Global Impression of Change (PGIC) after treatment. Surveys were given before treatment (baseline), after 6 and 12 weeks of treatment, and 6 weeks after the completion of stimulation sessions.
RESULTS:
The average total FSFI score across all subjects significantly increased from 15.3 ± 4.8 at baseline to 20.3 ± 7.8 after six sessions, 21.7 ± 7.5 after 12 sessions, and 21.3 ± 7.1 at study completion (p < 0.05 for all time points). Increases were observed in both DGNS and PTNS subjects. Significant FSFI increases were seen in the subdomains of lubrication, arousal, and orgasm, each of which is related to genital arousal. Bladder and general health surveys did not change across the study. PGIC had a significant increase. CONCLUSIONS: This study provides evidence that transcutaneous stimulation of peripheral nerves has the potential to be a valuable therapeutic tool for women with FSD. Be well! JP