Preventing Premature Births
April 1, 2009 Written by JP [Font too small?]Some compelling research was just presented at the Society for General Microbiology in Harrogate, England, the implications of which could impact the success rate for healthy births in women who might otherwise deliver prematurely. This same evidence may also reduce the risk of low birth-weight babies and infections in newborns.
Smile for Your Baby
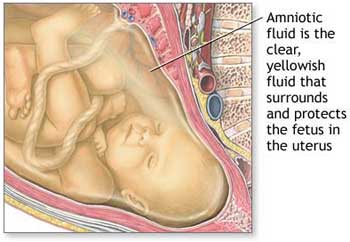
The basis for these findings comes from samples extracted from the amniotic fluid of 57 babies. In those samples researchers identified 46 species of bacteria. The vast majority of the bacteria were expected, in that they typically reside in the mother’s vagina. But there were two bacteria found (Granulicatella elegans and Streptococcus sinensis) that are specific to the mouth. The two bacteria in question are known to have the ability to enter the bloodstream and cause havoc in other areas of the body such as the heart.
 This hypothesis is strengthened by a Chinese review published in February, 2009. In that summary, researchers note a growing trend (in the past 10 years or so) between periodontitis (gum disease) and perinatal mortality (the period of time just before and after birth).
This hypothesis is strengthened by a Chinese review published in February, 2009. In that summary, researchers note a growing trend (in the past 10 years or so) between periodontitis (gum disease) and perinatal mortality (the period of time just before and after birth).
About 75% of preterm, low birth-weight (PLBW) are believed to be associated with maternal alcohol use, genetics, poor nutrition and prenatal care, smoking and urinary tract infections. But, that still leaves about a quarter of the PLBW cases with an undetermined cause. The authors of this review postulate that oral bacteria plays a role as the culprit in these instances. They believe that these pathogenic bacteria cause a cascade of inflammation that may provoke “spontaneous preterm labor and birth”.
The researchers involved conclude with the following statement, “oral health instruction and periodontal treatment may decrease the infection of periodontal pathogens and reduce the risk of PLBW. For the present, the best advice for a woman who contemplates pregnancy is effective brushing for two times per day and regular periodontal treatment.”
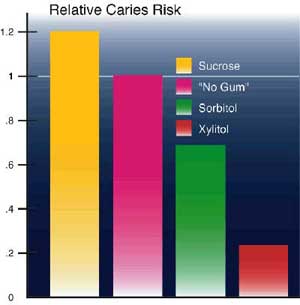
The advice given by the Chinese scientists is a good start. But I like the added suggestion given in a 2008 review in the journal of the American Family Physician. There they recommend using xylitol as a complementary treatment for two reasons. “Xylitol … may be used as adjuvant therapy for high-risk mothers in the early postpartum period to reduce transmission of carcinogenic bacteria to their infants. Appropriate dental care and prevention during pregnancy may reduce poor prenatal outcomes and decrease infant caries.”
In case you missed previous instances where I addressed the topic of dental health, here are a few blogs that provided information regarding other natural options for oral wellness:
- Green Tea and Periodontal Disease
- Natural Ingredients for a Healthy Smile
- Yogurt for Fresh Breath and Beyond
 Anything that adversely affects the health of an expectant mother also endangers the life inside of her. So in closing I’d like to share some brand new data from a study conducted in Ecuador. This trial focused on the role that CoQ10 (a powerful antioxidant) has in preventing pre-eclampsia (PE), a pregnancy related condition where the blood pressure of pregnant mothers becomes elevated to a dangerous level. It’s estimated that PE accounts for over 50,000 deaths per year worldwide.
Anything that adversely affects the health of an expectant mother also endangers the life inside of her. So in closing I’d like to share some brand new data from a study conducted in Ecuador. This trial focused on the role that CoQ10 (a powerful antioxidant) has in preventing pre-eclampsia (PE), a pregnancy related condition where the blood pressure of pregnant mothers becomes elevated to a dangerous level. It’s estimated that PE accounts for over 50,000 deaths per year worldwide.
The researchers involved found that women taking 200 mg daily of a CoQ10 soft gel had an 11% reduction in the risk of developing pre-eclampsia. The authors summarized these results in the following manner, “CoQ10 supplementation starting at 20 weeks of pregnancy appears to be a safe and well tolerated intervention, and resulted in a significant reduction in the rate of pre-eclampsia.”
Complications during pregnancy can often be prevented by following the common sense guidelines supported by most doctors. But there’s always emerging research that takes time to become integrated into the mainstream prenatal protocol. I hope that today’s blog will help those who are considering getting pregnant to increase the likelihood of the healthiest possible pregnancy for both mother and child.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
Be well!
JP
Tags: CoQ10, Pregnancy, Xylitol
Posted in Alternative Therapies, Dental Health, Women's Health

May 6th, 2015 at 3:46 pm
Update 05/06/15:
https://www.thieme-connect.com/DOI/DOI?10.1055/s-0035-1548835
Horm Metab Res. 2015 May 4.
Effects of High-Dose Vitamin D Supplementation on Metabolic Status and Pregnancy Outcomes in Pregnant Women at Risk for Pre-Eclampsia.
This study was designed to assess the beneficial effects of high-dose (cholecalciferol) vitamin D supplementation on metabolic profiles and pregnancy outcomes among pregnant women at risk for pre-eclampsia. This randomized double-blind placebo-controlled clinical trial was performed among 60 pregnant women at risk for pre-eclampsia according to abnormal uterine artery Doppler waveform. Subjects were randomly divided into 2 groups to receive 50 000 IU vitamin D supplements (n=30) or receive placebo (n=30) every 2 weeks from 20 to 32 weeks of gestation. Fasting blood samples were taken at baseline study and 12 weeks after the intervention to quantify relevant variables. Newborn’s anthropometric measurements were determined. Pregnant women who received cholecalciferol supplements had significantly increased serum 25-hydroxyvitamin D concentrations (+17.92±2.28 vs. +0.27±3.19 ng/ml, p<0.001) compared with the placebo. The administration of cholecalciferol supplements, compared with the placebo, resulted in significant differences in serum insulin concentrations (+1.08±6.80 vs. +9.57±10.32 μIU/ml, p<0.001), homeostasis model of assessment-insulin resistance (HOMA-IR) (+0.19±1.47 vs. +2.10±2.67, p<0.001), homeostatic model assessment-beta cell function (HOMA-B) (+5.82±29.58 vs. +39.81±38.00, p<0.001) and quantitative insulin sensitivity check index (QUICKI) score (-0.009±0.03 vs. -0.04±0.03, p=0.004). Furthermore, cholecalciferol-supplemented pregnant women had increased HDL-cholesterol concentrations (+2.67 ± 8.83 vs. -3.23±7.76 mg/dl, p=0.008) compared with the placebo. Finally, cholecalciferol supplementation led to a significant rise in plasma total antioxidant capacity (TAC) concentrations (+79.00±136.69 vs. -66.91±176.02 mmol/l, p=0.001) compared with the placebo. Totally, the administration of cholecalciferol supplements among pregnant women at risk for pre-eclampsia for 12 weeks had favorable effects on insulin metabolism parameters, serum HDL-cholesterol, and plasma TAC concentrations.
Be well!
JP
June 25th, 2015 at 7:31 pm
Update 06/25/15:
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=9795997&fileId=S000711451500166X
Br J Nutr. 2015 Jun 23:1-12.
The effect of zinc supplementation on pregnancy outcomes: a double-blind, randomised controlled trial, Egypt.
The present randomised controlled trial (RCT) was conducted to evaluate the effect of two regimens of Zn supplementation on pregnancy outcomes in Alexandria, Egypt. Healthy pregnant women aged 20-45 years and having low serum Zn level below the estimated median for the gestational age were eligible to participate in the trial. Of 1055 pregnant women assessed for the eligibility of low serum Zn level, 675 were eligible. These women were randomly assigned to one of the three groups: the Zn alone group (n 225) received a daily dose of 30 mg ZnSO4, the combined group (n 227) received 30 mg ZnSO4 plus multivitamins (B1, B6, D3, C and E) and the control group (n 223) received placebo (270 mg lactose). They were followed up from the time of recruitment till 1 week after delivery. Overall, there was no detectable difference in the mean birth weight between the three groups (mean 2929·12 (sd 330·28), 2922·22 (sd 324·05) and 2938·48 (sd 317·39) g for the placebo, Zn and Zn plus multivitamin groups, respectively, P= 0·88). Both the single and the combined Zn supplements were almost equally effective in reducing second- and third-stage complications (relative risk (RR) 0·43, 95 % CI 0·31, 0·60 for the Zn group and RR 0·54, 95 % CI 0·40, 0·73 for the combined group). Stillbirth and preterm delivery were significantly lower among the two supplemented groups than the placebo group (P= 0·001). Early neonatal morbidity was also significantly lower in the supplemented groups (RR 0·23, 95 % CI 0·15, 0·35 for the Zn group and RR 0·25, 95 % CI 0·16, 0·37 for the combined group). Collectively, Zn supplementation was effective in reducing pregnancy complications and early neonatal infection among the Zn-deficient women of the present trial.
Be well!
JP
January 17th, 2016 at 11:08 pm
Updated 1/17/16:
http://www.ejog.org/article/S0301-2115%2815%2900432-7/abstract
Eur J Obstet Gynecol Reprod Biol. 2015 Nov 30;198:40-46.
Effects of omega-3 fatty acids in prevention of early preterm delivery: a systematic review and meta-analysis of randomized studies.
OBJECTIVE: Preterm birth continues to be the one of the leading causes of infant deaths worldwide. There is a need for effective, easily available, safe and acceptable interventions to prevent preterm delivery, especially before 34 weeks of gestation. Omega-3 fatty acids such as EPA (eicosapentanoic acid) and DHA (docosahexanoic acid) are available as over the counter nutritional supplements, and are taken by women to improve pregnancy outcomes, without any clear recommendations. We undertook a systematic review to assess the effects of omega-3 fatty acids on early (<34 weeks) and any (<37 weeks) preterm delivery.
METHODS: We searched MEDLINE, EMBASE and Cochrane Library from inception to 2014 without any language restrictions. Study selection, quality assessment and data extraction were done by two independent reviewers. Results were summarized as relative risks and 95% confidence intervals for dichotomous outcomes and mean differences for continuous outcomes.
RESULTS: Of the nine included trials (5980 women), six (4193 women) evaluated the effects of omega-3 fatty acids on early preterm delivery. The risk of early preterm delivery was reduced by 58% (RR 0.42; 95% CI 0.27-0.66; I2=0%; p=0.0002) and any preterm delivery by 17% (RR 0.83; 95% CI 0.70-0.98; I2=0%; p=0.03) with the intervention. There was a significant increase in the mean gestational age by 1.95 weeks (95% CI 0.42-3.48 weeks; I2=0.47; p=0.01) and mean birth weight by 122.1g (95% CI 47.4-196.8; I2=0.84; p=0.001) in the intervention group compared to the controls. Subgroup analysis showed no significant differences in the effects between the groups according to the risk status, dose and timing of the intervention.
CONCLUSION: Omega-3 fatty acids are effective in preventing early and any preterm delivery. The intervention is simple and easily available and has the potential to influence population based strategies in the prevention of preterm birth.
Be well!
JP