Hemorrhagic Stroke Question
October 17, 2015 Written by JP [Font too small?]Recently, I was asked an intriguing question that regularly comes up in my line of work. A friend of the site wondered whether eating too many “super foods” or going overboard on supplements can increase the risk of hemorrhagic stroke. There are two types of stroke: hemorrhagic and ischemic. According to the National Stroke Association, only about 15% of strokes are the hemorrhagic variety. This form of stroke involves bleeding in the brain caused by damaged or weakened arteries and blood vessels. Cerebral blood spills build up pressure in the cranium and subsequently damage the brain.
Here’s where things get a bit complicated and interesting. If someone is at risk for cardiovascular disease, they are often prescribed aspirin or other medications that minimize the risk of abnormal blood clotting. If a clot blocks the flow of blood to the heart, a heart attack ensues. That same process causes an ischemic stroke (IS) when a clot prevents blood flow to the brain. However, while long-term use of aspirin can lower the risk of IS and myocardial infarctions, it actually increases the likelihood of hemorrhagic stroke (HS).
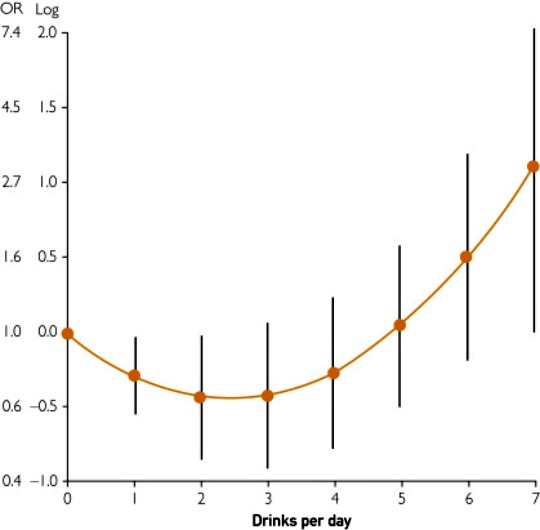
Many foods and supplements are known to possess “blood thinning” properties. There’s some evidence that over-consuming certain foods, such as alcohol, can predispose one to hemorrhagic episodes. Additionally, those with hereditary bleeding conditions may be more sensitive to these effects. For instance, those with a family history of hermorrhagic telangiectasia (nosebleeds) report that numerous foods seem to exacerbate this symptom. In an observational study, alcohol and spices topped the list. Other possible offenders included foods containing antiplatelet properties (garlic, ginger, ginseng) and salicylates (chocolate, coffee, red wine). It’s interesting to note that the active ingredient in aspirin is acetylsalicylic acid. See the connection?
Based on the information presented thus far, one could decide to avoid all of these conditionally beneficial foods just to be on the safe side. In most instances, I think that’s a mistake. Numerous studies have dismissed an association between the Mediterranean diet and HS. A Mediterranean eating pattern is rich in antioxidants, salicylates and various phytochemicals that influence circulation. Additionally, components of this dietary approach (fiber, fish, magnesium, potassium, Vitamin K) do not appear to increase HS risk. And, in some instances they may actually reduce it. One food that isn’t a traditional part of the Mediterranean, but bears consideration, is green tea. Drinking 3 cups of green tea has been shown to lower HS incidence by more than 20%.
When it comes to supplements, recent studies suggest that B-vitamins and multivitamins probably do little to harm or help the situation. On the other hand, supplemental vitamin E and ginkgo biloba extract may pose a threat of bleeding in susceptible individuals. This is especially relevant for those already using medications such as aspirin. Also, certain “supplements” intended to increase muscle mass and hasten weight loss have been linked to hemorraghic episodes. I strongly advise against using products containing dimethylamylamine (DMAA).
In closing, I want to circle back to the aspirin conundrum. While I can’t and don’t make any medical recommendations, I urge anyone concerned about aspirin side effects to consider an alternative: Pycnogenol. This well researched supplement promotes healthier circulation without increasing bleeding time. As a bonus, it may actually strengthen connective tissue. In theory, this could lessen the probability of blood vessel ruptures and tears. What’s more, preliminary research indicates that it’s better tolerated than aspirin.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Natural Stroke Association: Hemorrhagic Stroke … (link)
Study 2 – Aspirin for Primary Prevention of Cardiovascular Events … (link)
Study 3 – Lifestyle & Dietary Influences on Nosebleed Severity in Hereditary … (link)
Study 4 – Alcohol and Cardiovascular Health: The Dose Makes the Poison … (link)
Study 5 – A Mediterranean Diet & Risk of Myocardial Infarction, Heart Failure … (link)
Study 6 – Adherence to a Mediterranean diet and Prediction of Incident Stroke … (link)
Study 7 – Relation of the Traditional Mediterranean Diet to Cerebrovascular … (link)
Study 8 – Dietary Fiber Intake is Inversely Associated with Stroke Incidence … (link)
Study 9 – Total & Specific Fruit and Vegetable Consumption & Risk of Stroke … (link)
Study 10 – Total Antioxidant Capacity of Diet and Risk of Stroke: A Population … (link)
Study 11 – Association Between Intakes of Magnesium, Potassium, and Calcium … (link)
Study 12 – Intake of Dietary Phylloquinone & Menaquinones & Risk of Stroke … (link)
Study 13 – Long-Chain Omega-3 Polyunsaturated Fatty Acids and Risk of Stroke … (link)
Study 14 – Impact of Green Tea Consumption on the Prevention of Hemorrhagic … (link)
Study 15 – Tea Consumption & Risk of Cardiovascular Outcomes & Total Mortality … (link)
Study 16 – Multivitamin Use & Risk of Stroke Mortality: The Japan Collaborative … (link)
Study 17 – Vitamin B Supplementation, Homocysteine Levels, and the Risk of … (link)
Study 18 – Hemorrhagic Stroke in Young Healthy Male Following Use of Sports … (link)
Study 19 – Use of Recreational Drug 1,3 Dimethylamylamine (DMAA) … (link)
Study 20 – U.S. Food and Drug Administration: DMAA in Dietary Supplements … (link)
Study 21 – Ginkgo Biloba & Cerebral Bleeding: A Case Report & Critical Review … (link)
Study 22 – Does Ginkgo Biloba Reduce the Risk of Cardiovascular Events? … (link)
Study 23 – A Randomized Placebo-Controlled Trial of Ginkgo Biloba for the … (link)
Study 24 – Effects of Vitamin E on Stroke Subtypes: Meta-Analysis of Randomised … (link)
Study 25 – Vitamin E Serum Levels and Bleeding Risk in Patients Receiving Oral … (link)
Study 26 – Recurrence of Retinal Vein Thrombosis w/ Pycnogenol® or Aspirin® … (link)
Study 27 – Inhibition of Smoking-Induced Platelet Aggregation by Aspirin and … (link)
Study 28 – Pycnogenol Treatment of Acute Hemorrhoidal Episodes … (link)
High Alcohol Intake Increases Hemorrhagic Stroke Risk
Source: Mayo Clin Proc. 2014 Mar;89(3):382-93. (link)
Tags: Aspirin, Ginkgo Biloba, Stroke
Posted in Food and Drink, Heart Health, Nutritional Supplements


October 17th, 2015 at 4:27 pm
Updated 10/17/15:
https://www.jstage.jst.go.jp/article/jea/advpub/0/advpub_JE20150092/_pdf
J Epidemiol. 2015 Oct 10.
Coffee Consumption and Incidence of Subarachnoid Hemorrhage: The Jichi Medical School Cohort Study.
BACKGROUND: Previous studies on the association between coffee consumption and subarachnoid hemorrhage (SAH) have provided inconsistent results. We examine the risk of SAH from coffee consumption in a Japanese population.
METHODS: Our analyses were based on the Jichi Medical School Cohort Study, a large-scale population-based prospective cohort study. A total of 9941 participants (3868 men and 6073 women; mean age 55 years) with no history of cardiovascular disease or carcinoma were examined. Participants were asked to choose one of five options to indicate their daily coffee consumption: none, less than 1 cup a day, 1-2 cups a day, 3-4 cups a day, or 5 or more cups a day. The incidence of SAH was assessed independently by a diagnostic committee. Cox proportional hazards models were used to calculate hazard ratios (HRs) and their 95% confidence intervals (CI) after adjustment for age and sex (HR1) and for additional potential confounders (HR2).
RESULTS: During 10.7 years of follow-up, SAH occurred in 47 participants. When compared with the participants who consumed less than 1 cup of coffee a day, the HR of SAH was significantly higher in the group who consumed 5 or more cups a day in both models (HR1 4.49; 95% CI, 1.44-14.00; HR2 3.79; 95% CI, 1.19-12.05).
CONCLUSIONS: The present community-based cohort study showed that heavy coffee consumption was associated with an increased incidence of SAH after adjusting for age, sex, and multiple potential cardiovascular confounders.
Be well!
JP
October 17th, 2015 at 4:38 pm
Updated 10/17/15:
http://circ.ahajournals.org/content/131/8/721.long
Circulation. 2015 Feb 24;131(8):721-9.
Frequent physical activity may not reduce vascular disease risk as much as moderate activity: large prospective study of women in the United Kingdom.
BACKGROUND: Although physical activity has generally been associated with reduced risk of vascular disease, there is limited evidence about the effects of the frequency and duration of various activities on the incidence of particular types of vascular disease.
METHODS AND RESULTS: In 1998, on average, 1.1 million women without prior vascular disease reported their frequency of physical activity and many other personal characteristics. Three years later, they were asked about hours spent walking, cycling, gardening, and housework each week. Women were followed by record linkage to National Health Service cause-specific hospital admissions and death records. Cox regression was used to calculate adjusted relative risks for first vascular events in relation to physical activity. During an average of 9 years follow-up, 49,113 women had a first coronary heart disease event, 17,822 had a first cerebrovascular event, and 14,550 had a first venous thromboembolic event. In comparison with inactive women, those reporting moderate activity had significantly lower risks of all 3 conditions (P<0.001 for each). However, women reporting strenuous physical activity daily had higher risks of coronary heart disease (P=0.002), cerebrovascular disease (P<0.001), and venous thromboembolic events (P<0.001) than those reporting doing such activity 2 to 3 times per week. Risks did not differ between hemorrhagic and ischemic stroke, or between venous thromboembolic events with or without pulmonary embolism.
CONCLUSIONS: Moderate physical activity is associated with a lower risk of coronary heart disease, venous thromboembolic event, and cerebrovascular disease than inactivity. However, among active women, there is little to suggest progressive reductions in risk of vascular diseases with increasing frequency of activity.
Be well!
JP
October 17th, 2015 at 4:39 pm
Updated 10/17/15:
http://www.bmj.com/content/346/bmj.e8539.long
BMJ. 2013 Jan 7;346:e8539.
Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analysis of prospective cohort studies.
OBJECTIVE: To investigate and quantify the potential dose-response association between egg consumption and risk of coronary heart disease and stroke.
DESIGN: Dose-response meta-analysis of prospective cohort studies.
DATA SOURCES: PubMed and Embase prior to June 2012 and references of relevant original papers and review articles.
ELIGIBILITY CRITERIA FOR SELECTING STUDIES: Prospective cohort studies with relative risks and 95% confidence intervals of coronary heart disease or stroke for three or more categories of egg consumption.
RESULTS: Eight articles with 17 reports (nine for coronary heart disease, eight for stroke) were eligible for inclusion in the meta-analysis (3,081,269 person years and 5847 incident cases for coronary heart disease, and 4,148,095 person years and 7579 incident cases for stroke). No evidence of a curve linear association was seen between egg consumption and risk of coronary heart disease or stroke (P=0.67 and P=0.27 for non-linearity, respectively). The summary relative risk of coronary heart disease for an increase of one egg consumed per day was 0.99 (95% confidence interval 0.85 to 1.15; P=0.88 for linear trend) without heterogeneity among studies (P=0.97, I(2)=0%). For stroke, the combined relative risk for an increase of one egg consumed per day was 0.91 (0.81 to 1.02; P=0.10 for linear trend) without heterogeneity among studies (P=0.46, I(2)=0%). In a subgroup analysis of diabetic populations, the relative risk of coronary heart disease comparing the highest with the lowest egg consumption was 1.54 (1.14 to 2.09; P=0.01). In addition, people with higher egg consumption had a 25% (0.57 to 0.99; P=0.04) lower risk of developing hemorrhagic stroke.
CONCLUSIONS: Higher consumption of eggs (up to one egg per day) is not associated with increased risk of coronary heart disease or stroke. The increased risk of coronary heart disease among diabetic patients and reduced risk of hemorrhagic stroke associated with higher egg consumption in subgroup analyses warrant further studies.
Be well!
JP
October 31st, 2015 at 3:38 pm
Updated 10/31/15:
http://link.springer.com/article/10.1007%2Fs40520-015-0473-6
Aging Clin Exp Res. 2015 Oct 26.
Oily fish consumption is inversely correlated with cerebral microbleeds in community-dwelling older adults: results from the Atahualpa Project.
BACKGROUND: Oily fish is a major dietary source of omega-3 polyunsaturated fatty acids (ω-3 PUFAs). These nutrients improve endothelial dysfunction, reduce β-amyloid induced damage of neurovascular units, and might prevent the occurrence of cerebral microbleeds. However, this relationship has not been investigated so far.
AIM: To evaluate the association between oily fish intake and cerebral microbleeds in a population of frequent fish consumers living in coastal Ecuador.
METHODS: Cerebral microbleeds were identified by gradient-echo MRI and oily fish consumption was calculated in community-dwellers aged ≥60 years enrolled in the Atahualpa Project. The association between cerebral microbleeds and fish servings was examined in regression models adjusted for relevant confounders. A predictive model was constructed using quintiles of fish servings to take into account the non-linearity in the relationship.
RESULTS: Out of 311 eligible individuals, 293 (94 %) were enrolled. Cerebral microbleeds were recognized in 37 (13 %) individuals. Mean fish consumption was 8.8 ± 5.4 servings per week (ω-3 PUFAs estimates: 10.2 ± 7.1 g). Multivariate analysis showed an inverse relationship between cerebral microbleeds and fish consumption (p < 0.001). Predictive margins of CMB were higher for individuals in the lowest (≤4.3) than for those in the highest (≥13.1) quintile of fish servings (17.4 vs 2.3 %, p < 0.001). CONCLUSIONS: This study shows a lower cerebral microbleed presence among older adults eating large amounts of oily fish (13 servings per week, equivalent to about 15 g of ω-3 PUFAs). These high requirements can be more readily accomplished in other populations by taking fish oil preparations. Longitudinal studies are warranted to assess whether these interventions reduce incident cerebral microbleeds in high-risk individuals. Be well! JP
November 6th, 2015 at 11:38 am
Your article not only opened my eyes to the benefits of Pycnogenol but also how disciplined decisions on consuming a modest number of high alcohol drink can help reduce your risk of hemorrhagic stroke! It is fascinating to find how your research expands our knowledge.
I wish your articles found broad exposure through the media so many seniors could reap their wisdom!
I will recommend to read it to all my friends!
Thank you!
November 6th, 2015 at 11:41 am
Thank you, Paul! I wish for the same! 🙂
Be well!
JP
January 3rd, 2016 at 12:01 am
Updated 1/2/16:
http://jn.nutrition.org/content/145/8/1787.abstract
J Nutr. 2015 Aug;145(8):1787-92.
Choline and Betaine Intakes Are Not Associated with Cardiovascular Disease Mortality Risk in Japanese Men and Women.
BACKGROUND: Dietary intakes of betaine and choline may reduce the risk of cardiovascular disease; however, epidemiologic evidence is limited. Seafood is a rich source of betaine and is a popular traditional food in Japan.
OBJECTIVE: We examined the associations of betaine and choline intakes with cardiovascular disease mortality in a population-based cohort study in Japan.
METHODS: Study subjects were 13,355 male and 15,724 female residents of Takayama City, Japan, who were aged ≥35 y and enrolled in 1992. Their diets were assessed by a validated food frequency questionnaire. Deaths from coronary heart disease and stroke were identified from death certificates over 16 y. Multivariable-adjusted HRs were computed by using Cox regression models.
RESULTS: During follow-up, we documented 308 deaths from coronary heart disease and 676 deaths from stroke (393 from ischemic and 153 from hemorrhagic strokes). Compared with the lowest quartile, the second, third, and highest quartiles of betaine intake were significantly associated with a decreased risk of mortality from coronary heart disease in men after controlling for covariates. The HRs were 0.58 (95% CI: 0.36, 0.93), 0.62 (95% CI: 0.39, 0.998), and 0.60 (95% CI: 0.37, 0.97), respectively. The trend was not statistically significant (P = 0.08). There was no significant association between betaine intake and the risk of mortality from ischemic stroke. In women, betaine intake was unrelated risk of mortality from coronary heart disease and stroke (P = 0.32 and 0.73, respectively, for interaction by sex). There was no significant association between choline intake and cardiovascular disease mortality risk in men or women.
CONCLUSION: Overall, we found no clear evidence of significant associations between choline and betaine intakes and cardiovascular disease mortality risk in Japanese men and women.
Be well!
JP
June 26th, 2016 at 9:02 pm
Updated 06/26/16:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908235/
Evid Based Complement Alternat Med. 2016;2016:2795915.
Effectiveness of Gotu Kola Extract 750 mg and 1000 mg Compared with Folic Acid 3 mg in Improving Vascular Cognitive Impairment after Stroke.
This study aimed to determine the effectiveness of gotu kola (Centella asiatica) in improving cognitive function in patients with vascular cognitive impairment (VCI). This study uses a quasi-experimental design. Subjects in this study were patients with poststroke cognitive impairment who were treated at two hospitals in Yogyakarta, Indonesia. The number of subjects was 48: 17 subjects were treated with 1000 mg/day of gotu kola extract, 17 subjects treated with 750 mg/day of gotu kola extract, and 14 subjects treated with 3 mg/day of folic acid for 6 weeks. A Montreal Cognitive Assessment-Indonesian version (MoCA-Ina) was conducted at the beginning of treatment and after 6 weeks of therapy. It was found that all trials effectively improved poststroke VCI based on MoCA-Ina scores over the course of the study. There is no significant difference in ΔMoCA-Ina (score at the 6th week of treatment – score at the beginning) mean score among the three groups, indicating that gotu kola is as effective as folic acid in improving poststroke VCI. Gotu kola was shown to be more effective than folic acid in improving memory domain. This study suggested that gotu kola extract is effective in improving cognitive function after stroke.
Be well!
JP
February 27th, 2017 at 1:36 pm
Updated 02/27/17:
https://www.ncbi.nlm.nih.gov/pubmed/28237802
Neurosci Lett. 2017 Feb 22.
Early hyperbaric oxygen therapy may improve the long term neurological consequences of diabetic patients suffering from hemorrhagic stroke.
BACKGROUND: Hyperbaric oxygen therapy (HBOT) is still a controversial alternative strategy for acute stroke. This study was conducted to evaluate the potential long-term efficacy and safety of using HBOT in diabetes patients with intracerebral hemorrhage (ICH).
METHODS: In this randomized, prospective, normobaric oxygen therapy (NBOT)-controlled pilot study, 79 diabetes patients suffering from acute ICH were randomized to treat for 60minutes in a monoplace hyperbaric chamber pressurized with 100% O2 to 2.5-atm absolute (ATA) in the HBOT group or 1.5 ATA in the NBOT group. The primary outcomes included percentage of patients with improvement at one month and six months after onset (National Institutes of Health Stroke Scale [NIHSS], Barthel Index, modified Rankin Scale [mRS], Glasgow Outcome Scale [GOS]). The complications of all patients were recorded as well at the final follow-up of six months after onset.
RESULTS: Baseline characteristics were similar in both groups. There were no statistical differences between two groups at one month. However, in the long-term follow-up of six months, a larger percentage of patients in the HBOT group had a good outcome defined by their stroke scores compared with the HBOT group (Barthel Index: 85.1% versus 65.6%, P=0.080; mRS: 89.4% versus 68.8%, P=0.045; GOS: 83.0% versus 62.5%, P=0.073; NIHSS: 80.9% versus 56.2%, P=0.035).
CONCLUSIONS: In this study, early HBOT was found to be safe and effective with regards to the long term neurological consequences of diabetic patients suffering from ICH.
Be well!
JP