Kegel Exercises for Men
July 25, 2012 Written by JP [Font too small?]To some extent, symptoms of an enlarged prostate plague the majority of older men. In fact, if you’re male and fortunate enough to live a long life, you can almost certainly count on more frequent trips to the loo at night. Unfortunately, this isn’t the only potential consequence of benign prostatic hyperplasia (BPH). Many senior men also experience urinary urgency during their waking hours. What’s more, conventional and natural remedies don’t always provide satisfactory relief. But, Kegel exercises or Kegels are a free, safe and well researched option which work in conjunction with other treatments to greatly improve urinary dysfunction in this rapidly growing population.
A weak urinary sphincter is usually found in men with BPH, which prevents normal bladder contraction and function. Kegel exercises help to strengthen muscles that lie beneath the bladder which are essential for normal urinary control. Identifying the muscles in question can be accomplished quite simply by slowing down or stopping the flow of urine during urination. Once the exact muscles are located, one can contract them at any point during the day or night. In general, a set of 10 Kegels 3 to 4 times daily, is recommended. More detailed instructions can be found in the first three reference links below.
It’s important to note that Kegel exercises are serious medicine. Studies in numerous, prestigious medical journals report that Kegels improve bladder function and quality of life in patients with a variety of bladder disorders. The publications indicate that daily Kegel exercises benefit everyone from children with “daytime wetting” issues to men who have undergone radical prostatectomies. There’s also a long, positive track record for Kegels in women who develop urinary incontinence after childbirth or post-menopause. From my perspective, the primary stumbling block in the widespread implementation of Kegel exercises is the requirement for consistency. In order for muscles to strengthen and remain strong, you must exercise them as a course of habit. If Kegels are performed in this manner, the results can be quite predictable and pronounced. I highly recommend this underutilized practice to clients and anyone with issues relating to bladder control.
Note: Please check out the “Comments & Updates” section of this blog – at the bottom of the page. You can find the latest research about this topic there!
To learn more about the studies referenced in today’s column, please click on the following links:
Study 1 – Kegel Exercises: Treating Male Urinary Incontinence … (link)
Study 2 – Kegel Exercises for Men: Understand the Benefits … (link)
Study 3 – The 4-3-2 Method for Kegel Exercises … (link)
Study 4 – Efficacy of an Assisted Low-Intensity Programme of … (link)
Study 5 – Effectiveness of Early Pelvic Floor Rehabilitation Treatment … (link)
Study 6 – Pelvic Muscle Rehabilitation in Males Following Prostatectomy … (link)
Study 7 – Managing Urinary Incontinence in Community-Residing Elderly … (link)
Study 8 – Impact of a Health Education Intervention in Overactive Bladder … (link)
Study 9 – Long-Term Efficacy of Simple Behavioral Therapy for Daytime … (link)
Study 10 – Pelvic Floor Muscle Retraining for Pediatric Voiding Dysfunction … (link)
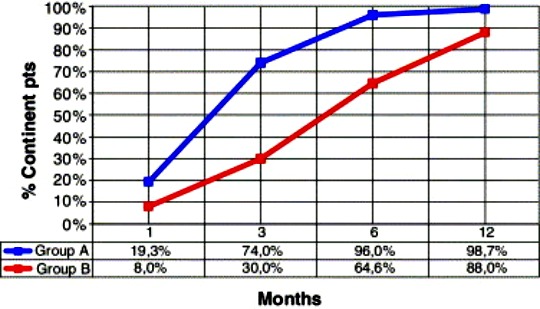
Kegel Exercises Improve Post-Prostatectomy Incontinence
Source: Eur Urol. 2005 Nov;48(5):734-8. (link)
Tags: aging, Incontinence, Prostate
Posted in Alternative Therapies, Exercise, Men's Health


March 27th, 2015 at 2:27 pm
Update: Pilates supports urinary continence after prostate surgery …
http://www.ncbi.nlm.nih.gov/pubmed/25809925
Neurourol Urodyn. 2015 Mar 21.
Is pilates as effective as conventional pelvic floor muscle exercises in the conservative treatment of post-prostatectomy urinary incontinence? A randomised controlled trial.
AIMS: To verify the efficacy of a Pilates exercise program compared to conventional pelvic floor muscle exercise (PFME) protocol in the conservative treatment of post-prostatectomy urinary incontinence (PPUI).
METHODS: Baseline assessment was performed four weeks postoperatively and included 24 hr pad test, bladder diary, and the ICIQ-SF. Patients were randomised into three groups: Pilates (G1), PFME combined with anal electrical stimulation (G2), and a control group (G3). Both treatment groups had to perform 10 weekly treatment sessions. Primary outcomes were mean reduction of daily pads and mean reduction of ICIQ-SF score four months after surgery. The significance level was set at P < 0.05. RESULTS: 85 patients completed the study. Differences between treatment groups (G1 and G2) in terms of mean reduction in daily pad usage, 24 hr pad test, and ICIQ-SF scores were not statistically significant (P > 0.05). The control group differed from G1 in daily pad usage (P = 0.01) and ICIQ-SF score (P = 0.0073). Intergroup comparisons revealed that 57.7% of the volunteers in G1 and 50% of the individuals from G2 no longer used pads by the end of the treatment period (P = 0.57). In the control group, 22.6% were not using pads four months after surgery, with statistical difference compared to G1 (P < 0.05). CONCLUSIONS: The Pilates exercise program proved to be as effective as conventional PFME to speed up continence recovery in PPUI. It also achieved a higher rate of fully continent patients when compared to the control group in the short-term. Be well! JP
April 6th, 2015 at 6:39 pm
Update: Kegel exercises improve continence after prostate surgery …
http://www.ncbi.nlm.nih.gov/pubmed/25065090
J Med Assoc Thai. 2014 May;97(5):513-7.
Effects of adding concentration therapy to Kegel exercise to improve continence after radical prostatectomy, randomized control.
OBJECTIVE: To compare the efficacy of pelvic floor muscle exercise with the concentration therapy versus pelvic floor muscle exercise alone after radical prostatectomy.
MATERIAL AND METHOD: One hundred thirty five patients were randomized into the intervention group that concentration therapy was added to Kegel exercise, and control group that was Kegel exercise only, using the stratified randomization (stratified by taking the catheter off before and after discharge) and type of surgery. Incontinence was defined as a loss of urine equal or more than to 2 grams in one-hour pad test, before and after the test in each sample group. Follow-up results were obtained by phone visit at 3, 4, 5, 6, 8, 10, and 12 weeks after surgery
RESULTS: In the intervention group, 65 of 68 cases (95.6%) had continence in three months, compared to 48 of 67 (71.6%) in the control group, with significant statistical difference (p-value < 0.001). The secondary result was the regularity in practicing. It was 80% in total. In the intervention group, 66 of 68 cases (97.06%) practiced compared to 34 of 67 (50.75%) in the control group, which was significant difference between the two groups. CONCLUSION: Combined concentration therapy with Kegel exercise had significantly improved continence after radical prostatectomy. Be well! JP
February 3rd, 2018 at 8:38 pm
Updated 2/3/18:
https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/s12906-018-2101-4
BMC Complement Altern Med. 2018 Jan 31;18(1):42.
Urox containing concentrated extracts of Crataeva nurvala stem bark, Equisetum arvense stem and Lindera aggregata root, in the treatment of symptoms of overactive bladder and urinary incontinence: a phase 2, randomised, double-blind placebo controlled trial.
BACKGROUND: Storage lower urinary tract symptoms (LUTS) including overactive bladder (OAB) and urinary incontinence (UI) affect millions of people worldwide, significantly impacting quality of life. Plant based medicines have been documented both empirically and in emerging scientific research to have varying benefits in reducing bladder symptoms. We assessed the efficacy of Urox®, a proprietary combination of phytomedicine extracts including, Cratevox™ (Crataeva nurvala) stem bark, Equisetem arvense stem and Lindera aggregata root, in reducing symptoms of OAB and UI.
METHODS: Efficacy of the herbal combination on a variety of bladder symptoms compared to an identical placebo, were documented in a randomised, double-blind, placebo controlled trial conducted at two primary care centres. Data were collected at baseline, 2, 4 and 8 weeks, with the primary outcome being self-reported urinary frequency. Statistical analysis included mixed effects ordered logistic regression with post hoc Holm’s test to account for repeated measures, and included an intention-to-treat analysis.
RESULTS: One hundred and fifty participants (59% female, aged; mean ± SD; 63.5 ± 13.1 years) took part in the study. At week 8, urinary day frequency was significantly lower (OR 0.01; 95%CI 0.01 to 0.02; p < 0.001) in response to treatment (mean ± SD; 7.69 ± 2.15/day) compared to placebo (10.95 ± 2.47/day). Similarly, episodes of nocturia were significantly fewer (OR 0.03; 95%CI 0.02 to 0.05) after 8 weeks of treatment (2.16 ± 1.49/night) versus placebo (3.14 ± 1.36/night). Symptoms of urgency (OR 0.02; 95%CI 0.01 to 0.03), and total incontinence (OR 0.03; 95% CI 0.01 to 0.06) were also lower (all p < 0.01) in the treatment group. Significant improvements in quality of life were reported after treatment in comparison to placebo. No significant side effects were observed resulting in withdrawal from treatment. CONCLUSIONS: The outcome of this study demonstrated both statistical significance and clinical relevance in reducing symptoms of OAB, urinary frequency and/or urgency and incontinence. The demonstrated viability of the herbal combination to serve as an effective treatment, with minimal side-effects, warrants further longer term research and consideration by clinicians. Be well! JP